Posttraumatic stress disorder
| Posttraumatic stress disorder | |
|---|---|
 | |
Art therapy project created by a U.S. Marine with posttraumatic stress disorder | |
| Specialty | Psychiatry, clinical psychology |
| Symptoms | Disturbing thoughts, feelings, or dreams related to the event; mental or physical distress to trauma-related cues; efforts to avoid trauma-related situations; increased fight-or-flight response[1] |
| Complications | Suicide[2] |
| Duration | > 1 month[1] |
| Causes | Exposure to a traumatic event[1] |
| Diagnostic method | Based on symptoms[2] |
| Treatment | Counseling, medication[3] |
| Medication | Selective serotonin reuptake inhibitor[4] |
| Frequency | 8.7% (lifetime risk); 3.5% (12-month risk) (USA)[5] |
Posttraumatic stress disorder (PTSD)[note 1] is a mental disorder that can develop after a person is exposed to a traumatic event, such as sexual assault, warfare, traffic collisions, or other threats on a person's life.[1] Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in how a person thinks and feels, and an increase in the fight-or-flight response.[1][3] These symptoms last for more than a month after the event.[1] Young children are less likely to show distress, but instead may express their memories through play.[1] A person with PTSD is at a higher risk for suicide and intentional self-harm.[2][6]
Most people who have experienced a traumatic event will not develop PTSD.[2] People who experience interpersonal trauma (for example rape or child abuse) are more likely to develop PTSD, as compared to people who experience non-assault based trauma, such as accidents and natural disasters.[7] About half of people develop PTSD following rape.[2] Children are less likely than adults to develop PTSD after trauma, especially if they are under 10 years of age.[8] Diagnosis is based on the presence of specific symptoms following a traumatic event.[2]
Prevention may be possible when counselling is targeted at those with early symptoms but is not effective when provided to all trauma-exposed individuals whether or not symptoms are present.[2] The main treatments for people with PTSD are counselling (psychotherapy) and medication.[3][9]Antidepressants of the selective serotonin reuptake inhibitor type are the first-line medications for PTSD and result in benefit in about half of people.[4] These benefits are less than those seen with counselling.[2] It is unclear if using medications and counselling together has greater benefit.[2][10] Other medications do not have enough evidence to support their use, and in the case of benzodiazepines, may worsen outcomes.[11][12]
In the United States about 3.5% of adults have PTSD in a given year, and 9% of people develop it at some point in their life.[1] In much of the rest of the world, rates during a given year are between 0.5% and 1%.[1] Higher rates may occur in regions of armed conflict.[2] It is more common in women than men.[3] Symptoms of trauma-related mental disorders have been documented since at least the time of the ancient Greeks.[13] During the World Wars the condition was known under various terms including "shell shock" and "combat neurosis".[14] The term "posttraumatic stress disorder" came into use in the 1970s in large part due to the diagnoses of U.S. military veterans of the Vietnam War.[15] It was officially recognized by the American Psychiatric Association in 1980 in the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III).[16]
.mw-parser-output .toclimit-2 .toclevel-1 ul,.mw-parser-output .toclimit-3 .toclevel-2 ul,.mw-parser-output .toclimit-4 .toclevel-3 ul,.mw-parser-output .toclimit-5 .toclevel-4 ul,.mw-parser-output .toclimit-6 .toclevel-5 ul,.mw-parser-output .toclimit-7 .toclevel-6 ul{display:none}
Contents
1 Signs and symptoms
1.1 Associated medical conditions
2 Risk factors
2.1 Trauma
2.1.1 Intimate partner violence
2.1.2 War-related trauma
2.1.3 Unexpected death of a loved one
2.1.4 Life-threatening illness
2.1.5 Pregnancy-related trauma
2.2 Genetics
3 Pathophysiology
3.1 Neuroendocrinology
3.2 Neuroanatomy
4 Diagnosis
4.1 Screening and assessment
4.2 Diagnostic and statistical manual
4.3 International classification of diseases
4.4 Differential diagnosis
5 Prevention
5.1 Psychological debriefing
5.2 Risk-targeted interventions
6 Management
6.1 Counselling
6.1.1 Cognitive behavioral therapy
6.1.2 Eye movement desensitization and reprocessing
6.1.3 Interpersonal psychotherapy
6.2 Medication
6.2.1 Antidepressants
6.2.2 Benzodiazepines
6.2.3 Glucocorticoids
6.2.4 Cannabinoids
6.3 Other
6.3.1 Exercise, sport and physical activity
6.3.2 Play therapy for children
6.3.3 Military programs
7 Epidemiology
7.1 United States
7.1.1 Military combat
7.1.2 Man-made disasters
8 Veterans
8.1 United States
8.2 United Kingdom
8.3 Canada
9 History
10 Terminology
11 Research
11.1 Psychotherapy adjuncts
12 Notes
13 References
14 External links
Signs and symptoms

Service members use art to relieve PTSD symptoms.
Symptoms of PTSD generally begin within the first 3 months after the inciting traumatic event, but may not begin until years later.[1][3] In the typical case, the individual with PTSD persistently avoids trauma-related thoughts and emotions, and discussion of the traumatic event, and may even have amnesia of the event.[citation needed] However, the event is commonly relived by the individual through intrusive, recurrent recollections, dissociative episodes of reliving the trauma ("flashbacks"), and nightmares.[17] While it is common to have symptoms after any traumatic event, these must persist to a sufficient degree (i.e., causing dysfunction in life or clinical levels of distress) for longer than one month after the trauma to be classified as PTSD (clinically significant dysfunction or distress for less than one month after the trauma may be acute stress disorder).[1][18][19][20] Some following a traumatic event experience posttraumatic growth.[21]
Associated medical conditions
Trauma survivors often develop depression, anxiety disorders, and mood disorders in addition to PTSD.[22]
Drug abuse and alcohol abuse commonly co-occur with PTSD.[23] Recovery from posttraumatic stress disorder or other anxiety disorders may be hindered, or the condition worsened, when substance use disorders are comorbid with PTSD. Resolving these problems can bring about improvement in an individual's mental health status and anxiety levels.[24][25]
In children and adolescents, there is a strong association between emotional regulation difficulties (e.g. mood swings, anger outbursts, temper tantrums) and post-traumatic stress symptoms, independent of age, gender, or type of trauma.[26]
Risk factors

No quieren (They do not want to) by Francisco Goya (1746–1828) depicts an elderly woman wielding a knife in defense of a girl being assaulted by a soldier.[27]
Persons considered at risk include combat military personnel, victims of natural disasters, concentration camp survivors, and victims of violent crime. Persons employed in occupations that expose them to violence (such as soldiers) or disasters (such as emergency service workers) are also at risk.[28] Other occupations that are at higher risk include police officers, firefighters, ambulance personnel, health care professionals, train drivers, divers, journalists, and sailors, in addition to people who work at banks, post offices or in stores.[29] The size of the hippocampus is inversely related to post-traumatic stress disorder and treatment success; the smaller the hippocampus, the higher risk of PTSD.[30]
Trauma
PTSD has been associated with a wide range of traumatic events. The risk of developing PTSD after a traumatic event varies by trauma type[31][32] and is highest following exposure to sexual violence (11.4%), particularly rape (19.0%).[33] Men are more likely to experience a traumatic event, but women are more likely to experience the kind of high-impact traumatic event that can lead to PTSD, such as interpersonal violence and sexual assault.[34]
Motor vehicle collision survivors, both children and adults, are at an increased risk of PTSD.[35][36] About 20% of children were diagnosed with PTSD following a road traffic accident, compared to 22% of adults.[35][36] Females were more likely to be diagnosed with PTSD following a road traffic accident, whether the accident occurred during childhood or adulthood.[35][36]
Posttraumatic stress reactions have not been studied as well in children and adolescents as adults.[8] The rate of PTSD may be lower in children than adults, but in the absence of therapy, symptoms may continue for decades.[8] One estimate suggests that the proportion of children and adolescents having PTSD in a non-wartorn population in a developed country may be 1% compared to 1.5% to 3% of adults, and much lower below the age of 10 years.[8] On average, 16% of children exposed to a traumatic event develop PTSD, varying according to type of exposure and gender.[37] Similar to the adult population, risk factors for PTSD in children include: female gender, exposure to disasters (natural or manmade), negative coping behaviours, and/or lacking proper social support systems.[38]
Predictor models have consistently found that childhood trauma, chronic adversity, and familial stressors increase risk for PTSD as well as risk for biological markers of risk for PTSD after a traumatic event in adulthood.[39][40][41] Experiencing bullying as a child or an adult has been correlated with the development of PTSD.[42] Peritraumatic dissociation in children is a predictive indicator of the development of PTSD later in life.[43] This effect of childhood trauma, which is not well understood, may be a marker for both traumatic experiences and attachment problems.[44][45] Proximity to, duration of, and severity of the trauma make an impact, and interpersonal traumas cause more problems than impersonal ones.[46]
The risk of developing PTSD is increased in individuals who are exposed to physical abuse, physical assault, or kidnapping.[47][48] Women who experience physical violence are more likely to develop PTSD than men.[47]
Intimate partner violence
An individual that has been exposed to domestic violence is predisposed to the development of PTSD. However, being exposed to a traumatic experience does not automatically indicate that an individual will develop PTSD.[49] There is a strong association between the development of PTSD in mothers that experienced domestic violence during the perinatal period of their pregnancy.[50]
Those who have experienced sexual assault or rape may develop symptoms of PTSD.[51][52] PTSD symptoms include re-experiencing the assault, avoiding things associated with the assault, numbness, and increased anxiety and an increased startle response. The likelihood of sustained symptoms of PTSD is higher if the rapist confined or restrained the person, if the person being raped believed the rapist would kill him or her, the person who was raped was very young or very old, and if the rapist was someone he or she knew. The likelihood of sustained severe symptoms is also higher if people around the survivor ignore (or are ignorant of) the rape or blame the rape survivor.[53]
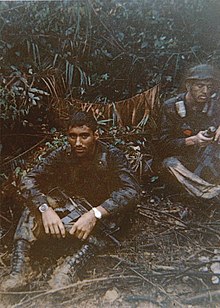
A U.S. Long-Range Patrol team leader in Vietnam, 1968.
Military service is a risk factor for developing PTSD.[54] Around 78% of people exposed to combat do not develop PTSD; in about 25% of military personnel who develop PTSD, its appearance is delayed.[54]
Refugees are also at an increased risk for PTSD due to their exposure to war, hardships, and traumatic events. The rates for PTSD within refugee populations range from 4% to 86%.[55] While the stresses of war impact everyone involved, displaced persons have been shown to be more affected than nondisplaced persons.[56]
Unexpected death of a loved one
Sudden, unexpected death of a loved one is the most common traumatic event type reported in cross-national studies.[33][57] However, the majority of people who experience this type of event will not go on to develop PTSD. An analysis from the WHO World Mental Health Surveys found a 5.2% risk of developing PTSD after learning of the unexpected death of a loved one.[57] Because of the high prevalence of this type of traumatic event, unexpected death of a loved one accounts for approximately 20% of PTSD cases worldwide.[33]
Life-threatening illness
Medical conditions associated with an increased risk of PTSD include cancer,[58][59][60] heart attack,[61] and stroke.[62] 22% of cancer survivors present with lifelong PTSD like symptoms.[63] Intensive-care unit (ICU) hospitalization is also a risk factor for PTSD.[64] Some women experience PTSD from their experiences related to breast cancer and mastectomy.[65][66][58] Loved ones of those who experience life-threatening illnesses are also at risk for developing PTSD, such as parents of child with chronic illnesses.[67]
Women who experience miscarriage are at risk of PTSD.[68][69][70] Those who experience subsequent miscarriages have an increased risk of PTSD compared to those experiencing only one.[68] PTSD can also occur after childbirth and the risk increases if a woman has experienced trauma prior to the pregnancy.[71][72] Prevalence of PTSD following normal childbirth (that is, excluding stillbirth or major complications) is estimated to be between 2.8 and 5.6% at 6 weeks postpartum,[73] with rates dropping to 1.5% at 6 months postpartum.[73][74] Symptoms of PTSD are common following childbirth, with prevalence of 24-30.1%[73] at 6 weeks, dropping to 13.6% at 6 months.[75] Emergency childbirth is also associated with PTSD.[76] Some women experience PTSD from their experiences related to breast cancer and mastectomy.[65][66][58]
Genetics
There is evidence that susceptibility to PTSD is hereditary. Approximately 30% of the variance in PTSD is caused from genetics alone.[43] For twin pairs exposed to combat in Vietnam, having a monozygotic (identical) twin with PTSD was associated with an increased risk of the co-twin's having PTSD compared to twins that were dizygotic (non-identical twins).[77] There is evidence that those with a genetically smaller hippocampus are more likely to develop PTSD following a traumatic event. Research has also found that PTSD shares many genetic influences common to other psychiatric disorders. Panic and generalized anxiety disorders and PTSD share 60% of the same genetic variance. Alcohol, nicotine, and drug dependence share greater than 40% genetic similarities.[43]
Several biological indicators have been identified that are related to later PTSD development. Heightened startle responses and a smaller hippocampal volume have been identified as biomarkers for the risk of developing PTSD.[30] Additionally, one study found that soldiers whose leukocytes had greater numbers of glucocorticoid receptors were more prone to developing PTSD after experiencing trauma.[78]
Pathophysiology
Neuroendocrinology
PTSD symptoms may result when a traumatic event causes an over-reactive adrenaline response, which creates deep neurological patterns in the brain. These patterns can persist long after the event that triggered the fear, making an individual hyper-responsive to future fearful situations.[18][79] During traumatic experiences the high levels of stress hormones secreted suppress hypothalamic activity that may be a major factor toward the development of PTSD.[80]
PTSD causes biochemical changes in the brain and body, that differ from other psychiatric disorders such as major depression. Individuals diagnosed with PTSD respond more strongly to a dexamethasone suppression test than individuals diagnosed with clinical depression.[81][82]
Most people with PTSD show a low secretion of cortisol and high secretion of catecholamines in urine,[83] with a norepinephrine/cortisol ratio consequently higher than comparable non-diagnosed individuals.[84] This is in contrast to the normative fight-or-flight response, in which both catecholamine and cortisol levels are elevated after exposure to a stressor.[85]
Brain catecholamine levels are high,[86] and corticotropin-releasing factor (CRF) concentrations are high.[87][88] Together, these findings suggest abnormality in the hypothalamic-pituitary-adrenal (HPA) axis.
The maintenance of fear has been shown to include the HPA axis, the locus coeruleus-noradrenergic systems, and the connections between the limbic system and frontal cortex. The HPA axis that coordinates the hormonal response to stress,[89] which activates the LC-noradrenergic system, is implicated in the over-consolidation of memories that occurs in the aftermath of trauma.[90] This over-consolidation increases the likelihood of one's developing PTSD. The amygdala is responsible for threat detection and the conditioned and unconditioned fear responses that are carried out as a response to a threat.[43]
The HPA axis is responsible for coordinating the hormonal response to stress.[43] Given the strong cortisol suppression to dexamethasone in PTSD, HPA axis abnormalities are likely predicated on strong negative feedback inhibition of cortisol, itself likely due to an increased sensitivity of glucocorticoid receptors.[91]
PTSD has been hypothesized to be a maladaptive learning pathway to fear response through a hypersensitive, hyperreactive, and hyperresponsive HPA axis.[92]
Low cortisol levels may predispose individuals to PTSD: Following war trauma, Swedish soldiers serving in Bosnia and Herzegovina with low pre-service salivary cortisol levels had a higher risk of reacting with PTSD symptoms, following war trauma, than soldiers with normal pre-service levels.[93] Because cortisol is normally important in restoring homeostasis after the stress response, it is thought that trauma survivors with low cortisol experience a poorly contained—that is, longer and more distressing—response, setting the stage for PTSD.
It is thought that the locus coeruleus-noradrenergic system mediates the over-consolidation of fear memory. High levels of cortisol reduce noradrenergic activity, and because people with PTSD tend to have reduced levels of cortisol, it has been proposed that individuals with PTSD cannot regulate the increased noradrenergic response to traumatic stress.[80] Intrusive memories and conditioned fear responses are thought to be a result of the response to associated triggers. Neuropeptide Y has been reported to reduce the release of norepinephrine and has been demonstrated to have anxiolytic properties in animal models. Studies have shown people with PTSD demonstrate reduced levels of NPY, possibly indicating their increased anxiety levels.[43]
Other studies indicate that people that suffer from PTSD have chronically low levels of serotonin, which contributes to the commonly associated behavioral symptoms such as anxiety, ruminations, irritability, aggression, suicidality, and impulsivity.[94] Serotonin also contributes to the stabilization of glucocorticoid production.
Dopamine levels in a person with PTSD can contribute to symptoms: low levels can contribute to anhedonia, apathy, impaired attention, and motor deficits; high levels can contribute to psychosis, agitation, and restlessness.[94]
Multiple studies described elevated concentrations of the thyroid hormone triiodothyronine in PTSD.[95] This kind of type 2 allostatic adaptation may contribute to increased sensitivity to catecholamines and other stress mediators.
Hyperresponsiveness in the norepinephrine system can also be caused by continued exposure to high stress. Overactivation of norepinephrine receptors in the prefrontal cortex can be connected to the flashbacks and nightmares frequently experienced by those with PTSD. A decrease in other norepinephrine functions (awareness of the current environment) prevents the memory mechanisms in the brain from processing that the experience, and emotions the person is experiencing during a flashback are not associated with the current environment.[94]
There is considerable controversy within the medical community regarding the neurobiology of PTSD. A 2012 review showed no clear relationship between cortisol levels and PTSD. The majority of reports indicate people with PTSD have elevated levels of corticotropin-releasing hormone, lower basal cortisol levels, and enhanced negative feedback suppression of the HPA axis by dexamethasone.[43][96]
Neuroanatomy
Regions of the brain associated with stress and posttraumatic stress disorder[97]
A meta-analysis of structural MRI studies found an association with reduced total brain volume, intracranial volume, and volumes of the hippocampus, insula cortex, and anterior cingulate.[98] Much of this research stems from PTSD in those exposed to the Vietnam War.[99][100]
People with PTSD have decreased brain activity in the dorsal and rostral anterior cingulate cortices and the ventromedial prefrontal cortex, areas linked to the experience and regulation of emotion.[101]
The amygdala is strongly involved in forming emotional memories, especially fear-related memories. During high stress, the hippocampus, which is associated with placing memories in the correct context of space and time and memory recall, is suppressed. According to one theory this suppression may be the cause of the flashbacks that can affect people with PTSD. When someone with PTSD undergoes stimuli similar to the traumatic event, the body perceives the event as occurring again because the memory was never properly recorded in the person's memory.[43][102]
The amygdalocentric model of PTSD proposes that the amygdala is very much aroused and insufficiently controlled by the medial prefrontal cortex and the hippocampus, in particular during extinction.[103] This is consistent with an interpretation of PTSD as a syndrome of deficient extinction ability.[103][104]
The basolateral nucleus (BLA) of the amygdala is responsible for the comparison and development of associations between unconditioned and conditioned responses to stimuli, which results in the fear conditioning present in PTSD. The BLA activates the central nucleus (CeA) of the amygdala, which elaborates the fear response, (including behavioral response to threat and elevated startle response). Descending inhibitory inputs from the medial prefrontal cortex (mPFC) regulate the transmission from the BLA to the CeA, which is hypothesized to play a role in the extinction of conditioned fear responses.[43] While as a whole, amygdala hyperactivity is reported by meta analysis of functional neuroimaging in PTSD, there is a large degree of heterogeniety, more so than in social anxiety disorder or phobic disorder. Comparing dorsal(roughly the CeA) and ventral(roughly the BLA) clusters, hyperactivity is more robust in the ventral cluster, while hypoactivity is evident in the dorsal cluster. The distinction may explain the blunted emotions in PTSD(via desensitization in the CeA) as well as the fear related component.[105]
In a 2007 study Vietnam War combat veterans with PTSD showed a 20% reduction in the volume of their hippocampus compared with veterans having suffered no such symptoms.[106] This finding was not replicated in chronic PTSD patients traumatized at an air show plane crash in 1988 (Ramstein, Germany).[107]
Diagnosis
PTSD can be difficult to diagnose, because of:
- the subjective nature of most of the diagnostic criteria (although this is true for many mental disorders);
- the potential for over-reporting, e.g., while seeking disability benefits, or when PTSD could be a mitigating factor at criminal sentencing;
- the potential for under-reporting, e.g., stigma, pride, fear that a PTSD diagnosis might preclude certain employment opportunities;
- symptom overlap with other mental disorders such as obsessive compulsive disorder and generalized anxiety disorder;[108]
- association with other mental disorders such as major depressive disorder and generalized anxiety disorder;
- substance use disorders, which often produce some of the same signs and symptoms as PTSD; and
- substance use disorders can increase vulnerability to PTSD or exacerbate PTSD symptoms or both; and
- PTSD increases the risk for developing substance abuse disorders.
- the differential expression of symptoms culturally (specifically with respect to avoidance and numbing symptoms, distressing dreams, and somatic symptoms)[109]
Screening and assessment
A number of screening instruments are used for screening adults for PTSD, such as the PTSD Checklist for DSM-5 (PCL-5)[110][111] and the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5).[112]
There are also several screening and assessment instruments for use with children and adolescents. These include the Child PTSD Symptom Scale (CPSS),[113][114] Child Trauma Screening Questionnaire,[115][116] and UCLA Posttraumatic Stress Disorder Reaction Index for DSM-IV.[117][118]
In addition, there are also screening and assessment instruments for caregivers of very young children (six years of age and younger). These include the Young Child PTSD Screen,[119] the Young Child PTSD Checklist,[119] and the Diagnostic Infant and Preschool Assessment.[120]
Diagnostic and statistical manual
PTSD was classified as an anxiety disorder in the DSM-IV, but has since been reclassified as a "trauma- and stressor-related disorder" in the DSM-5.[1] The DSM-5 diagnostic criteria for PTSD include four symptom clusters: re-experiencing, avoidance, negative alterations in cognition/mood, and alterations in arousal and reactivity.[1][3]
International classification of diseases
The International Classification of Diseases and Related Health Problems 10 (ICD-10) classifies PTSD under "Reaction to severe stress, and adjustment disorders."[121] The ICD-10 criteria for PTSD include re-experiencing, avoidance, and either increased reactivity or inability to recall certain details related to the event.[121]
The ICD-11 diagnostic description for PTSD contains three components or symptom groups (1) re-experiencing, (2) avoidance, and (3) heightened sense of threat.[122][123] Another difference between the ICD-10 and ICD-11 PTSD diagnostic formulations, ICD-11 no longer includes verbal thoughts about the traumatic event as a symptom.[123] There is a predicted lower rate of diagnosed PTSD using ICD-11 compared to ICD10 or DSM-5.[123] ICD-11 also proposes identifying a distinct group with complex post-traumatic stress disorder (CPTSD), who have more often experienced multiple and sustained traumas and have greater functional impairment than those with PTSD. [123]
Differential diagnosis
A diagnosis of PTSD requires that the person has been exposed to an extreme, life-threatening stressor. Any stressor can result in a diagnosis of adjustment disorder and it is an appropriate diagnosis for a stressor and a symptom pattern that does not meet the criteria for PTSD.
The symptom pattern for acute stress disorder must occur and be resolved within four weeks of the trauma. If it lasts longer, and the symptom pattern fits that characteristic of PTSD, the diagnosis may be changed.[17]
Obsessive compulsive disorder may be diagnosed for intrusive thoughts that are recurring but not related to a specific traumatic event.[17]
In extreme cases of prolonged, repeated traumatization where there is no viable chance of escape, survivors may develop complex post-traumatic stress disorder.[124] This occurs as a result of layers of trauma rather than a single traumatic event, and includes additional symptomatology, such as the loss of a coherent sense of self.[125]
Prevention
Modest benefits have been seen from early access to cognitive behavioral therapy. Critical incident stress management has been suggested as a means of preventing PTSD, but subsequent studies suggest the likelihood of its producing negative outcomes.[126][127] A review "...did not find any evidence to support the use of an intervention offered to everyone", and that "...multiple session interventions may result in worse outcome than no intervention for some individuals."[128] The World Health Organization recommends against the use of benzodiazepines and antidepressants in those having experienced trauma.[129] Some evidence supports the use of hydrocortisone for prevention in adults, although there is limited or no evidence supporting propranolol, escitalopram, temazepam, or gabapentin.[130]
Psychological debriefing
Trauma-exposed individuals often receive treatment called psychological debriefing in an effort to prevent PTSD, which consists of interviews that are meant to allow individuals to directly confront the event and share their feelings with the counselor and to help structure their memories of the event.[131] However, several meta-analyses find that psychological debriefing is unhelpful and is potentially harmful.[131][132][133] This is true for both single-session debriefing and multiple session interventions.[128] As of 2017 The American Psychological Association assessed psychological debriefing as No Research Support/Treatment is Potentially Harmful.[134]
Risk-targeted interventions
Risk-targeted interventions are those that attempt to mitigate specific formative information or events. It can target modeling normal behaviors, instruction on a task, or giving information on the event.[135][136]
Management
Reviews of studies have found that combination therapy (psychological and pharmacotherapy) is no more effective than psychological therapy alone.[10]
Counselling
The approaches with the strongest evidence include behavioral and cognitive-behavioral therapies such as prolonged exposure therapy,[137]cognitive processing therapy, and eye movement desensitization and reprocessing (EMDR).[138][139][140] In addition, brief eclectic psychotherapy (BEP), narrative exposure therapy (NET), and written narrative exposure therapies also have a evidence.[141]
A meta-analytic comparison of EMDR and cognitive behavioral therapy (CBT) found both protocols indistinguishable in terms of effectiveness in treating PTSD; however, "the contribution of the eye movement component in EMDR to treatment outcome" is unclear.[142] A meta-analysis in children and adolescent also found that EMDR was as efficacious as cognitive behavioral therapy.[143]
Furthermore, the availability of school-based therapy is particularly important for children with PTSD.[non sequitur] Children with PTSD are far more likely to pursue treatment at school (because of its proximity and ease) than at a free clinic.[144]
Cognitive behavioral therapy

The diagram depicts how emotions, thoughts, and behaviors all influence each other. The triangle in the middle represents CBT's tenet that all humans' core beliefs can be summed up in three categories: self, others, future.
CBT seeks to change the way a person feels and acts by changing the patterns of thinking or behavior, or both, responsible for negative emotions. CBT has been proven to be an effective treatment for PTSD and is currently considered the standard of care for PTSD by the United States Department of Defense.[145][146] In CBT, individuals learn to identify thoughts that make them feel afraid or upset and replace them with less distressing thoughts. The goal is to understand how certain thoughts about events cause PTSD-related stress.[147][148]
Recent research on contextually based third-generation behavior therapies suggests that they may produce results comparable to some of the better validated therapies.[149] Many of these therapy methods have a significant element of exposure[150] and have demonstrated success in treating the primary problems of PTSD and co-occurring depressive symptoms.[151]
Exposure therapy is a type of cognitive behavioral therapy[152] that involves assisting trauma survivors to re-experience distressing trauma-related memories and reminders in order to facilitate habituation and successful emotional processing of the trauma memory. Most exposure therapy programs include both imaginal confrontation with the traumatic memories and real-life exposure to trauma reminders; this therapy modality is well supported by clinical evidence.[citation needed] The success of exposure-based therapies has raised the question of whether exposure is a necessary ingredient in the treatment of PTSD.[153] Some organizations[which?] have endorsed the need for exposure.[154][155] The U.S. Department of Veterans Affairs has been actively training mental health treatment staff in prolonged exposure therapy[156] and Cognitive Processing Therapy[157] in an effort to better treat U.S. veterans with PTSD.
Eye movement desensitization and reprocessing
Eye movement desensitization and reprocessing (EMDR) is a form of psychotherapy developed and studied by Francine Shapiro.[158] She had noticed that, when she was thinking about disturbing memories herself, her eyes were moving rapidly. When she brought her eye movements under control while thinking, the thoughts were less distressing.[158]
In 2002, Shapiro and Maxfield published a theory of why this might work, called adaptive information processing.[159] This theory proposes that eye movement can be used to facilitate emotional processing of memories, changing the person's memory to attend to more adaptive information.[160] The therapist initiates voluntary rapid eye movements while the person focuses on memories, feelings or thoughts about a particular trauma.[8][161] The therapists uses hand movements to get the person to move their eyes backward and forward, but hand-tapping or tones can also be used.[8] EMDR closely resembles cognitive behavior therapy as it combines exposure (re-visiting the traumatic event), working on cognitive processes and relaxation/self-monitoring.[8] However, exposure by way of being asked to think about the experience rather than talk about it has been highlighted as one of the more important distinguishing elements of EMDR.[162]
There have been multiple small controlled trials of four to eight weeks of EMDR in adults[163] as well as children and adolescents.[161] EMDR reduced PTSD symptoms enough in the short term that one in two adults no longer met the criteria for PTSD, but the number of people involved in these trials was small and thus results should be interpreted with caution pending further research.[163] There was not enough evidence to know whether or not EMDR could eliminate PTSD in adults.[163] In children and adolescents, a recent meta-analysis of randomized controlled trials using MetaNSUE to avoid biases related to missing information found that EMDR was at least as efficacious as CBT, and superior to waitlist or placebo.[143] There was some evidence that EMDR might prevent depression.[163] There were no studies comparing EMDR to other psychological treatments or to medication.[163] Adverse effects were largely unstudied.[163] The benefits were greater for women with a history of sexual assault compared with people who had experienced other types of traumatizing events (such as accidents, physical assaults and war). There is a small amount of evidence that EMDR may improve re-experiencing symptoms in children and adolescents, but EMDR has not been shown to improve other PTSD symptoms, anxiety, or depression.[161]
The eye movement component of the therapy may not be critical for benefit.[8][160] As there has been no major, high quality randomized trial of EMDR with eye movements versus EMDR without eye movements, the controversy over effectiveness is likely to continue.[162] Authors of a meta-analysis published in 2013 stated, "We found that people treated with eye movement therapy had greater improvement in their symptoms of post-traumatic stress disorder than people given therapy without eye movements....Secondly we found that that in laboratory studies the evidence concludes that thinking of upsetting memories and simultaneously doing a task that facilitates eye movements reduces the vividness and distress associated with the upsetting memories."[139]
Interpersonal psychotherapy
Other approaches, in particular involving social supports,[164][165] may also be important. An open trial of interpersonal psychotherapy[166] reported high rates of remission from PTSD symptoms without using exposure.[167] A current, NIMH-funded trial in New York City is now (and into 2013) comparing interpersonal psychotherapy, prolonged exposure therapy, and relaxation therapy.[168][full citation needed][169][170]
Medication
While many medications do not have enough evidence to support their use, three (fluoxetine, paroxetine, and venlafaxine) have been shown to have a small benefit over placebo.[12] With many medications, residual PTSD symptoms following treatment is the rule rather than the exception.[171]
Antidepressants
Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) may have some benefit for PTSD symptoms.[12][172]Tricyclic antidepressants are equally effective but are less well tolerated.[173] Evidence provides support for a small or modest improvement with sertraline, fluoxetine, paroxetine, and venlafaxine.[12][174] Thus, these four medications are considered to be first-line medications for PTSD.[172][4]
Benzodiazepines
Benzodiazepines are not recommended for the treatment of PTSD due to a lack of evidence of benefit and risk of worsening PTSD symptoms.[175] Some authors believe that the use of benzodiazepines is contraindicated for acute stress, as this group of drugs can cause dissociation.[176] Nevertheless, some use benzodiazepines with caution for short-term anxiety and insomnia.[177][178][179] While benzodiazepines can alleviate acute anxiety, there is no consistent evidence that they can stop the development of PTSD and may actually increase the risk of developing PTSD 2–5 times.[11] Additionally, benzodiazepines may reduce the effectiveness of psychotherapeutic interventions, and there is some evidence that benzodiazepines may actually contribute to the development and chronification of PTSD. For those who already have PTSD, benzodiazepines may worsen and prolong the course of illness, by worsening psychotherapy outcomes, and causing or exacerbating aggression, depression (including suicidality), and substance use.[11] Drawbacks include the risk of developing a benzodiazepine dependence, tolerance (i.e., short-term benefits wearing off with time), and withdrawal syndrome; additionally, individuals with PTSD (even those without a history of alcohol or drug misuse) are at an increased risk of abusing benzodiazepines.[4][180] Due to a number of other treatments with greater efficacy for PTSD and less risks (e.g., prolonged exposure, cognitive processing therapy, eye movement desensitization and reprocessing, cognitive restructuring therapy, trauma-focused cognitive behavioral therapy, brief eclectic psychotherapy, narrative therapy, stress inoculation training, serotonergic antidepressants, adrenergic inhibitors, antipsychotics, and even anticonvulsants), benzodiazepines should be considered relatively contraindicated until all other treatment options are exhausted.[9][181] For those who argue that benzodiazepines should be used sooner in the most severe cases, the adverse risk of disinhibition (associated with suicidality, aggression and crimes) and clinical risks of delaying or inhibiting definitive efficacious treatments, make other alternative treatments preferable (e.g., inpatient, residential, partial hospitalization, intensive outpatient, dialectic behavior therapy; and other fast-acting sedating medications such as trazodone, mirtazapine, amitripytline, doxepin, prazosin, propranolol, guanfacine, clonidine, quetiapine, olanzapine, valproate, gabapentin).[4][181][182]
Glucocorticoids
Glucocorticoids may be useful for short-term therapy to protect against neurodegeneration caused by the extended stress response that characterizes PTSD, but long-term use may actually promote neurodegeneration.[183]
Cannabinoids
Evidence as of 2017 is insufficient to determine if medical cannabis is useful for PTSD.[184] Despite the uncertain evidence, use of cannabis or derived products is widespread among U.S. veterans with PTSD.[185]
The cannabinoid nabilone is sometimes used off-label for nightmares in PTSD. Although some short-term benefit was shown, adverse effects are common and it has not been adequately studied to determine efficacy.[186] Additionally, there are other treatments with stronger efficacy and less risks (e.g., psychotherapy, serotonergic antidepressants, adrenergic inhibitors). The use of medical marijuana for PTSD is controversial, with only a handful of states permitting its use for that purpose.[187]
Other
Exercise, sport and physical activity
Physical activity can influence people's psychological[188] and physical health.[189] The U.S. National Center for PTSD recommends moderate exercise as a way to distract from disturbing emotions, build self-esteem and increase feelings of being in control again. They recommend a discussion with a doctor before starting an exercise program.[190]
Play therapy for children
Play is thought to help children link their inner thoughts with their outer world, connecting real experiences with abstract thought.[191] Repetitive play can also be one way a child relives traumatic events, and that can be a symptom of trauma in a child or young person.[192] Although it is commonly used, there have not been enough studies comparing outcomes in groups of children receiving and not receiving play therapy, so the effects of play therapy are not yet understood.[8][191]
Military programs
Many veterans of the wars in Iraq and Afghanistan have faced significant physical, emotional, and relational disruptions. In response, the United States Marine Corps has instituted programs to assist them in re-adjusting to civilian life, especially in their relationships with spouses and loved ones, to help them communicate better and understand what the other has gone through.[193]Walter Reed Army Institute of Research (WRAIR) developed the Battlemind program to assist service members avoid or ameliorate PTSD and related problems. Wounded Warrior Project partnered with the US Department of Veterans Affairs to create Warrior Care Network, a national health system of PTSD treatment centers.[194][195]
Epidemiology

Disability-adjusted life year rates for posttraumatic stress disorder per 100,000 inhabitants in 2004.[196].mw-parser-output .refbegin{font-size:90%;margin-bottom:0.5em}.mw-parser-output .refbegin-hanging-indents>ul{list-style-type:none;margin-left:0}.mw-parser-output .refbegin-hanging-indents>ul>li,.mw-parser-output .refbegin-hanging-indents>dl>dd{margin-left:0;padding-left:3.2em;text-indent:-3.2em;list-style:none}.mw-parser-output .refbegin-100{font-size:100%}
no data
< 43.5
43.5–45
45–46.5
46.5–48
48–49.5
49.5–51
51–52.5
52.5–54
54–55.5
55.5–57
57–58.5
> 58.5
There is debate over the rates of PTSD found in populations, but, despite changes in diagnosis and the criteria used to define PTSD between 1997 and 2013, epidemiological rates have not changed significantly.[197][198] Most of the current reliable data regarding the epidemiology of PTSD is based on DSM-IV criteria, as the DSM-5 was not introduced until 2013.
The United Nations' World Health Organization publishes estimates of PTSD impact for each of its member states; the latest data available are for 2004. Considering only the 25 most populated countries ranked by overall age-standardized Disability-Adjusted Life Year (DALY) rate, the top half of the ranked list is dominated by Asian/Pacific countries, the US, and Egypt.[199] Ranking the countries by the male-only or female-only rates produces much the same result, but with less meaningfulness, as the score range in the single-sex rankings is much-reduced (4 for women, 3 for men, as compared with 14 for the overall score range), suggesting that the differences between female and male rates, within each country, is what drives the distinctions between the countries.[200][201]
As of 2017, the cross-national lifetime prevalence of PTSD was 3.9%, based on a survey were 5.6% had been exposed to trauma.[202] The primary factor impacting treatment-seeking behavior, which can help to mitigate PTSD development after trauma was income, while being younger, female, and having less social status (less education, lower individual income, and being unemployed) were all factors associated with less treatment-seeking behaviour.[202]
| Region | Country | PTSD DALY rate, overall[199] | PTSD DALY rate, females[200] | PTSD DALY rate, males[201] |
|---|---|---|---|---|
| Asia / Pacific | Thailand | 59 | 86 | 30 |
| Asia / Pacific | Indonesia | 58 | 86 | 30 |
| Asia / Pacific | Philippines | 58 | 86 | 30 |
| Americas | USA | 58 | 86 | 30 |
| Asia / Pacific | Bangladesh | 57 | 85 | 29 |
| Africa | Egypt | 56 | 83 | 30 |
| Asia / Pacific | India | 56 | 85 | 29 |
| Asia / Pacific | Iran | 56 | 83 | 30 |
| Asia / Pacific | Pakistan | 56 | 85 | 29 |
| Asia / Pacific | Japan | 55 | 80 | 31 |
| Asia / Pacific | Myanmar | 55 | 81 | 30 |
| Europe | Turkey | 55 | 81 | 30 |
| Asia / Pacific | Vietnam | 55 | 80 | 30 |
| Europe | France | 54 | 80 | 28 |
| Europe | Germany | 54 | 80 | 28 |
| Europe | Italy | 54 | 80 | 28 |
| Asia / Pacific | Russian Federation | 54 | 78 | 30 |
| Europe | United Kingdom | 54 | 80 | 28 |
| Africa | Nigeria | 53 | 76 | 29 |
| Africa | Dem. Republ. of Congo | 52 | 76 | 28 |
| Africa | Ethiopia | 52 | 76 | 28 |
| Africa | South Africa | 52 | 76 | 28 |
| Asia / Pacific | China | 51 | 76 | 28 |
| Americas | Mexico | 46 | 60 | 30 |
| Americas | Brazil | 45 | 60 | 30 |
United States
The National Comorbidity Survey Replication has estimated that the lifetime prevalence of PTSD among adult Americans is 6.8%, with women (9.7%) more than twice as likely as men[94] (3.6%) to have PTSD at some point in their lives.[47] More than 60% of men and more than 60% of women experience at least one traumatic event in their life. The most frequently reported traumatic events by men are rape, combat, and childhood neglect or physical abuse. Women most frequently report instances of rape, sexual molestation, physical attack, being threatened with a weapon and childhood physical abuse.[94] 88% of men and 79% of women with lifetime PTSD have at least one comorbid psychiatric disorder. Major depressive disorder, 48% of men and 49% of women, and lifetime alcohol abuse or dependence, 51.9% of men and 27.9% of women, are the most common comorbid disorders.[203]
Military combat
The United States Department of Veterans Affairs estimates that 830,000 Vietnam War veterans suffered symptoms of PTSD.[204] The National Vietnam Veterans' Readjustment Study (NVVRS) found 15.2% of male and 8.5% of female Vietnam veterans to suffer from current PTSD at the time of the study. Life-Time prevalence of PTSD was 30.9% for males and 26.9% for females. In a reanalysis of the NVVRS data, along with analysis of the data from the Matsunaga Vietnam Veterans Project, Schnurr, Lunney, Sengupta, and Waelde found that, contrary to the initial analysis of the NVVRS data, a large majority of Vietnam veterans suffered from PTSD symptoms (but not the disorder itself). Four out of five reported recent symptoms when interviewed 20–25 years after Vietnam.[205]
A 2011 study from Georgia State University and San Diego State University found that rates of PTSD diagnosis increased significantly when troops were stationed in combat zones, had tours of longer than a year, experienced combat, or were injured. Military personnel serving in combat zones were 12.1 percentage points more likely to receive a PTSD diagnosis than their active-duty counterparts in non-combat zones. Those serving more than 12 months in a combat zone were 14.3 percentage points more likely to be diagnosed with PTSD than those having served less than one year. Experiencing an enemy firefight was associated a 18.3 percentage point increase in the probability of PTSD, while being wounded or injured in combat was associated a 23.9 percentage point increase in the likelihood of a PTSD diagnosis. For the 2.16 million U.S. troops deployed in combat zones between 2001 and 2010, the total estimated two-year costs of treatment for combat-related PTSD are between $1.54 billion and $2.69 billion.[206]
As of 2013, rates of PTSD have been estimated at up to 20% for veterans returning from Iraq and Afghanistan.[207] As of 2013 13% of veterans returning from Iraq were unemployed.[208]
Man-made disasters
The September 11 attacks took the lives of nearly 3,000 people, leaving 6,000 injured.[209] First responders (police and firefighters), emergency medical services, sanitation workers, and volunteers were all involved in the recovery efforts. The prevalence of probable PTSD in these highly exposed populations was estimated across multiple studies utilizing in-person, telephone, and online interviews and questionnaires.[209][210][211] Overall prevalence of PTSD was highest immediately following the attacks and decreased over time. However, disparities were found among the different types of recovery workers.[209][210] The rate of probable PTSD for first responders was lowest directly after the attacks and increased from ranges of 4.8-7.8% to 7.4-16.5% between the 5-6 year follow-up and a later assessment.[209] When comparing traditional responders to non-traditional responders (volunteers), the probable PTSD prevalence 2.5 years after the initial visit was greater in volunteers with estimates of 11.7% and 17.2% respectively.[209] Volunteer participation in tasks atypical to the defined occupational role was a significant risk factor for PTSD.[210] Other risk factors included exposure intensity, earlier start date, duration of time spent on site, and constant, negative reminders of the trauma.[209][210] Additional research has been performed to understand the social consequences of the September 11 attacks. Alcohol consumption was assessed in a cohort of World Trade Center workers using the cut-annoyed-guilty-eye (CAGE) questionnaire for alcohol abuse. Almost 50% of World Trade Center workers who self-identified as alcohol users reported drinking more during the rescue efforts.[211] Nearly a quarter of these individuals reported drinking more following the recovery.[211] If determined to have probable PTSD status, the risk of developing an alcohol problem was double compared to those without psychological morbidity.[211] Social disability was also studied in this cohort as a social consequence of the September 11 attacks. Defined by the disruption of family, work, and social life, the risk of developing social disability increased 17-fold when categorized as having probable PTSD.[211]
Veterans

Vietnam Veterans Memorial, Washington, D.C.
United States
The United States provides a range of benefits for veterans that the VA has determined have PTSD, which developed during, or as a result of, their military service. These benefits may include tax-free cash payments,[212] free or low-cost mental health treatment and other healthcare,[213] vocational rehabilitation services,[214] employment assistance,[215] and independent living support.[216][217]
United Kingdom
In the UK, there are various charities and service organisations dedicated to aiding veterans in readjusting to civilian life. The Royal British Legion and the more recently established Help for Heroes are two of Britain's more high-profile veterans' organisations which have actively advocated for veterans over the years. There has been some controversy that the NHS has not done enough in tackling mental health issues and is instead "dumping" veterans on charities such as Combat Stress.[218][219]
Canada
Veterans Affairs Canada offers a new program that includes rehabilitation, financial benefits, job placement, health benefits program, disability awards, peer support[220][221][222] and family support.[223]
History
The 1952 edition of the DSM-I includes a diagnosis of "gross stress reaction", which has similarities to the modern definition and understanding of PTSD.[224] Gross stress reaction is defined as a "normal personality [utilizing] established patterns of reaction to deal with overwhelming fear" as a response to "conditions of great stress".[225] The diagnosis includes language which relates the condition to combat as well as to "civilian catastrophe".[225]
Early in 1978, the term was used in a working group finding presented to the Committee of Reactive Disorders.[226] The condition was added to the DSM-III, which was being developed in the 1980s, as posttraumatic stress disorder.[224][226] In the DSM-IV, the spelling "posttraumatic stress disorder" is used, while in the ICD-10, the spelling is "post-traumatic stress disorder".[227]
The addition of the term to the DSM-III was greatly influenced by the experiences and conditions of U.S. military veterans of the Vietnam War.[228] Due to its association with the war in Vietnam, PTSD has become synonymous with many historical war-time diagnoses such as railway spine, stress syndrome, nostalgia, soldier's heart, shell shock, battle fatigue, combat stress reaction, or traumatic war neurosis.[229][230] Some of these terms date back to the 19th century, which is indicative of the universal nature of the condition. In a similar vein, psychiatrist Jonathan Shay has proposed that Lady Percy's soliloquy in the William Shakespeare play Henry IV, Part 1 (act 2, scene 3, lines 40–62[231]), written around 1597, represents an unusually accurate description of the symptom constellation of PTSD.[232]

Statue, Three Servicemen, Vietnam Veterans Memorial
The correlations between combat and PTSD are undeniable; according to Stéphane Audoin-Rouzeau and Annette Becker, "One-tenth of mobilized American men were hospitalized for mental disturbances between 1942 and 1945, and, after thirty-five days of uninterrupted combat, 98% of them manifested psychiatric disturbances in varying degrees."[233] In fact, much of the available published research regarding PTSD is based on studies done on veterans of the war in Vietnam. A study based on personal letters from soldiers of the 18th-century Prussian Army concludes that combatants may have had PTSD.[234] Aspects of PTSD in soldiers of ancient Assyria have been identified using written sources from 1300–600 BCE. These Assyrian soldiers would undergo a three-year rotation of combat before being allowed to return home, and were purported to have faced immense challenges in reconciling their past actions in war with their civilian lives.[235] Connections between the actions of Viking berserkers and the hyperarousal of post-traumatic stress disorder have also been drawn.[236]
The researchers from the Grady Trauma Project highlight the tendency people have to focus on the combat side of PTSD: "less public awareness has focused on civilian PTSD, which results from trauma exposure that is not combat related... " and "much of the research on civilian PTSD has focused on the sequelae of a single, disastrous event, such as the Oklahoma City bombing, September 11th attacks, and Hurricane Katrina".[237] Disparity in the focus of PTSD research affects the already popular perception of the exclusive interconnectedness of combat and PTSD. This is misleading when it comes to understanding the implications and extent of PTSD as a neurological disorder. Dating back to the definition of Gross stress reaction in the DSM-I, civilian experience of catastrophic or high stress events is included as a cause of PTSD in medical literature. The 2014 National Comorbidity Survey reports that "the traumas most commonly associated with PTSD are combat exposure and witnessing among men and rape and sexual molestation among women."[238]
Because of the initial overt focus on PTSD as a combat related disorder when it was first fleshed out in the years following the war in Vietnam, in 1975 Ann Wolbert Burgess and Lynda Lytle Holmstrom defined Rape trauma syndrome, RTS, in order to draw attention to the striking similarities between the experiences of soldiers returning from war and of rape victims.[239] This paved the way for a more comprehensive understanding of causes of PTSD.
After PTSD became an official psychiatric diagnosis with the publication of DSM-III (1980), the number of personal injury lawsuits (tort claims) asserting the plaintiff suffered from PTSD increased rapidly. However, triers of fact (judges and juries) often regarded the PTSD diagnostic criteria as imprecise, a view shared by legal scholars, trauma specialists, forensic psychologists, and forensic psychiatrists. Professional discussions and debates in academic journals, at conferences, and between thought leaders, led to a more clearly-defined set of diagnostic criteria in DSM-IV, particularly the definition of a "traumatic event".[240]
The DSM-IV classified PTSD under anxiety disorders, but the DSM-5 created a new category called "Trauma- and Stressor-Related Disorders," in which PTSD is now classified.[1]
Terminology
The Diagnostic and Statistical Manual of Mental Disorders does not hyphenate 'post' and 'traumatic', thus, the DSM-5 lists the disorder as posttraumatic stress disorder. However, many scientific journal articles and other scholarly publications do hyphenate the name of the disorder, viz., post-traumatic stress disorder.[241] Dictionaries also differ with regard to the preferred spelling of the disorder with the Collins English Dictionary - Complete and Unabridged using the hyphenated spelling, and the American Heritage Dictionary of the English Language, Fifth Edition and the Random House Kernerman Webster's College Dictionary giving the non-hyphenated spelling.[242]
Some at the Pentagon have used the terminology "PTSS" (syndrome instead of disorder, to avoid connotation of stigma), or just "PTS".[243]
Research
Most knowledge regarding PTSD comes from studies in high-income countries.[244]
To recapitulate some of the neurological and neurobehavioral symptoms experienced by the veteran population of recent conflicts in Iraq and Afghanistan, researchers at the Roskamp Institute and the James A Haley Veteran's Hospital (Tampa) have developed an animal model to study the consequences of mild traumatic brain injury (mTBI) and PTSD.[245] In the laboratory, the researchers exposed mice to a repeated session of unpredictable stressor (i.e. predator odor while restrained), and physical trauma in the form of inescapable foot-shock, and this was also combined with a mTBI. In this study, PTSD animals demonstrated recall of traumatic memories, anxiety, and an impaired social behavior, while animals subject to both mTBI and PTSD had a pattern of disinhibitory-like behavior. mTBI abrogated both contextual fear and impairments in social behavior seen in PTSD animals. In comparison with other animal studies,[245][246] examination of neuroendocrine and neuroimmune responses in plasma revealed a trend toward increase in corticosterone in PTSD and combination groups.
Psychotherapy adjuncts
MDMA was used for psychedelic therapy for a variety of indications before its criminalization in the U.S. in 1985. In response to its criminalization, the Multidisciplinary Association for Psychedelic Studies (MAPS) was founded as a nonprofit drug-development organization to develop MDMA into a legal prescription drug for use as an adjunct in psychotherapy.[247] The drug is hypothesized to facilitate psychotherapy by reducing fear, thereby allowing people to reprocess and accept their traumatic memories without becoming emotionally overwhelmed. In this treatment, people participate in an extended psychotherapy session during the acute activity of the drug, and then spend the night at the treatment facility. In the sessions with the drug, therapists are not directive and support the patients in exploring their inner experiences. People participate in standard psychotherapy sessions before the drug-assisted sessions, as well as after the drug-assisted psychotherapy to help them integrate their experiences with the drug.[248] The phase 2 clinical trials of the MDMA-Assisted Psychotherapy, was publicized at the end of November 2016.[249] Preliminary results suggest MDMA-assisted psychotherapy might be effective.[250] MAPS received FDA approval of a phase 3 trials.[251][252]
Researchers are also investigating using D-cycloserine, hydrocortisone, and propranolol as add on therapy to more conventional exposure therapy.[253]
Notes
^ Acceptable variants of this term exist; see the Terminology section in this article.
References
^ abcdefghijklmn American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. pp. 271–280. ISBN 978-0-89042-555-8..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output .citation q{quotes:"""""""'""'"}.mw-parser-output .citation .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .citation .cs1-lock-limited a,.mw-parser-output .citation .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .citation .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-ws-icon a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/4/4c/Wikisource-logo.svg/12px-Wikisource-logo.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-maint{display:none;color:#33aa33;margin-left:0.3em}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ abcdefghij Bisson JI, Cosgrove S, Lewis C, Robert NP (November 2015). "Post-traumatic stress disorder". BMJ. 351: h6161. doi:10.1136/bmj.h6161. PMC 4663500. PMID 26611143.
^ abcdef "Post-Traumatic Stress Disorder". National Institute of Mental Health. February 2016. Archived from the original on 9 March 2016. Retrieved 10 March 2016.
^ abcde Berger W, Mendlowicz MV, Marques-Portella C, Kinrys G, Fontenelle LF, Marmar CR, Figueira I (March 2009). "Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: a systematic review". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 33 (2): 169–80. doi:10.1016/j.pnpbp.2008.12.004. PMC 2720612. PMID 19141307.
^ Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association (5th ed.). Arlington, VA: American Psychiatric Association. 2013. p. 276. ISBN 9780890425558. OCLC 830807378.
^ Panagioti M, Gooding PA, Triantafyllou K, Tarrier N (April 2015). "Suicidality and posttraumatic stress disorder (PTSD) in adolescents: a systematic review and meta-analysis". Social Psychiatry and Psychiatric Epidemiology. 50 (4): 525–37. doi:10.1007/s00127-014-0978-x. PMID 25398198.
^ Zoladz PR, Diamond DM (June 2013). "Current status on behavioral and biological markers of PTSD: a search for clarity in a conflicting literature". Neuroscience and Biobehavioral Reviews. 37 (5): 860–95. doi:10.1016/j.neubiorev.2013.03.024. PMID 23567521.
^ abcdefghi National Collaborating Centre for Mental Health (UK) (2005). Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. NICE Clinical Guidelines, No. 26. National Institute for Health and Clinical Excellence: Guidance. Gaskell (Royal College of Psychiatrists). ISBN 9781904671251. Archived from the original on 2017-09-08. Lay summary – Pubmed Health (plain English).

^ ab Haagen JF, Smid GE, Knipscheer JW, Kleber RJ (August 2015). "The efficacy of recommended treatments for veterans with PTSD: A metaregression analysis". Clinical Psychology Review. 40: 184–94. doi:10.1016/j.cpr.2015.06.008. PMID 26164548.
^ ab Hetrick SE, Purcell R, Garner B, Parslow R (July 2010). "Combined pharmacotherapy and psychological therapies for post traumatic stress disorder (PTSD)". The Cochrane Database of Systematic Reviews (7): CD007316. doi:10.1002/14651858.CD007316.pub2. PMID 20614457.
^ abc Guina J, Rossetter SR, DeRHODES BJ, Nahhas RW, Welton RS (July 2015). "Benzodiazepines for PTSD: A Systematic Review and Meta-Analysis". Journal of Psychiatric Practice. 21 (4): 281–303. doi:10.1097/pra.0000000000000091. PMID 26164054.
^ abcd Hoskins M, Pearce J, Bethell A, Dankova L, Barbui C, Tol WA, van Ommeren M, de Jong J, Seedat S, Chen H, Bisson JI (February 2015). "Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis". The British Journal of Psychiatry. 206 (2): 93–100. doi:10.1192/bjp.bp.114.148551. PMID 25644881.Some drugs have a small positive impact on PTSD symptoms
^ Carlstedt R (2009). Handbook of Integrative Clinical Psychology, Psychiatry, and Behavioral Medicine Perspectives, Practices, and Research. New York: Springer Pub. Co. p. 353. ISBN 9780826110954.
^ Herman J (2015). Trauma and Recovery: The Aftermath of Violence—From Domestic Abuse to Political Terror. Basic Books. p. 9. ISBN 9780465098736.
^ Klykylo WM (2012). Clinical child psychiatry (3. ed.). Chichester, West Sussex, UK: John Wiley & Sons. p. Chapter 15. ISBN 9781119967705.
^ Friedman MJ (October 2013). "Finalizing PTSD in DSM-5: getting here from there and where to go next". Journal of Traumatic Stress. 26 (5): 548–56. doi:10.1002/jts.21840. PMID 24151001.
^ abc American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: American Psychiatric Association. ISBN 978-0-89042-061-4.
[page needed]; on-line.
^ ab Rothschild, Babette (2000). The Body Remembers: The Psychophysiology of Trauma and Trauma Treatment. New York: W.W. Norton & Company. ISBN 978-0-393-70327-6.
[page needed]
^ Kaplan HI, Sadock BJ (1994). Grebb JA, ed. Kaplan and Sadock's synopsis of psychiatry: Behavioral sciences, clinical psychiatry (7th ed.). Baltimore: Williams & Williams. pp. 606–609.
[page needed]
^ Satcher D (1999). "Chapter 4". Mental Health: A Report of the Surgeon General. Surgeon General of the United States. Archived from the original on 2010-07-02.
^ Bernstein, M; Pfefferbaum, B (16 May 2018). "Posttraumatic Growth as a Response to Natural Disasters in Children and Adolescents". Current Psychiatry Reports. 20 (5): 37. doi:10.1007/s11920-018-0900-4. PMID 29766312.
^ O'Donnell ML, Creamer M, Bryant RA, Schnyder U, Shalev A (July 2003). "Posttraumatic disorders following injury: an empirical and methodological review". Clinical Psychology Review. 23 (4): 587–603. doi:10.1016/S0272-7358(03)00036-9. PMID 12788111.
^ Maxmen JS, Ward NG (2002). Psychotropic drugs: fast facts (3rd ed.). New York: W. W. Norton. p. 348. ISBN 978-0-393-70301-6.
^ Cohen SI (February 1995). "Alcohol and benzodiazepines generate anxiety, panic and phobias". Journal of the Royal Society of Medicine. 88 (2): 73–7. PMC 1295099. PMID 7769598.
^ Spates R, Souza T (2007). "Treatment of PTSD and Substance Abuse Comorbidity" (PDF). The Behavior Analyst Today. 9 (1): 11–26. doi:10.1037/h0100643. Archived from the original (PDF) on 23 June 2014.
^ Villalta L, Smith P, Hickin N, Stringaris A (April 2018). "Emotion regulation difficulties in traumatized youth: a meta-analysis and conceptual review". European Child & Adolescent Psychiatry. 27 (4): 527–544. doi:10.1007/s00787-018-1105-4. PMID 29380069.
^ Robinson, Maisah (May 27, 2006). "Review of Francisco Goya's Disasters of War". Associated Press. Archived from the original on 2014-07-28.
[unreliable source?]
^ Fullerton CS, Ursano RJ, Wang L (August 2004). "Acute stress disorder, posttraumatic stress disorder, and depression in disaster or rescue workers". The American Journal of Psychiatry. 161 (8): 1370–6. CiteSeerX 10.1.1.600.4486. doi:10.1176/appi.ajp.161.8.1370. PMID 15285961.
^ Skogstad M, Skorstad M, Lie A, Conradi HS, Heir T, Weisæth L (April 2013). "Work-related post-traumatic stress disorder". Occupational Medicine. 63 (3): 175–82. doi:10.1093/occmed/kqt003. PMID 23564090. Archived from the original on 2016-07-25. Retrieved 2016-07-15.
^ ab Yamasue H, Kasai K, Iwanami A, Ohtani T, Yamada H, Abe O, Kuroki N, Fukuda R, Tochigi M, Furukawa S, Sadamatsu M, Sasaki T, Aoki S, Ohtomo K, Asukai N, Kato N (July 2003). "Voxel-based analysis of MRI reveals anterior cingulate gray-matter volume reduction in posttraumatic stress disorder due to terrorism". Proceedings of the National Academy of Sciences of the United States of America. 100 (15): 9039–43. Bibcode:2003PNAS..100.9039Y. doi:10.1073/pnas.1530467100. PMC 166434. PMID 12853571.
^ Vieweg WV, Julius DA, Fernandez A, Beatty-Brooks M, Hettema JM, Pandurangi AK (May 2006). "Posttraumatic stress disorder: clinical features, pathophysiology, and treatment". The American Journal of Medicine. 119 (5): 383–90. doi:10.1016/j.amjmed.2005.09.027. PMID 16651048.
^ "Trauma and Posttraumatic Stress Disorder". Massachusetts General Hospital comprehensive clinical psychiatry. Stern, Theodore A.,, Massachusetts General Hospital. (Second ed.). London: Elsevier. 2016. pp. 380–392. ISBN 9780323295079. OCLC 905232521.
^ abc Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV, Ferry F, Florescu S, Gureje O, Haro JM, Huang Y, Karam EG, Kawakami N, Lee S, Lepine JP, Levinson D, Navarro-Mateu F, Pennell BE, Piazza M, Posada-Villa J, Scott KM, Stein DJ, Ten Have M, Torres Y, Viana MC, Petukhova MV, Sampson NA, Zaslavsky AM, Koenen KC (2017-10-27). "Trauma and PTSD in the WHO World Mental Health Surveys". European Journal of Psychotraumatology. 8 (sup5): 1353383. doi:10.1080/20008198.2017.1353383. PMC 5632781. PMID 29075426.
^ National Collaborating Centre for Mental Health (UK) (2005). Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. NICE Clinical Guidelines, No. 26. National Institute for Health and Clinical Excellence: Guidance. Gaskell (Royal College of Psychiatrists). ISBN 9781904671251. Archived from the original on 2017-09-08. Lay summary – Pubmed Health (plain English).

^ abc Lin W, Gong L, Xia M, Dai W (January 2018). "Prevalence of posttraumatic stress disorder among road traffic accident survivors: A PRISMA-compliant meta-analysis". Medicine. 97 (3): e9693. doi:10.1097/md.0000000000009693. PMC 5779792. PMID 29505023.
^ abc Dai W, Liu A, Kaminga AC, Deng J, Lai Z, Wen SW (August 2018). "Prevalence of Posttraumatic Stress Disorder among Children and Adolescents following Road Traffic Accidents: A Meta-Analysis". Canadian Journal of Psychiatry. 63 (12): 798–808. doi:10.1177/0706743718792194. PMC 6309043. PMID 30081648.
^ Alisic E, Zalta AK, van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, Smid GE (2014). "Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis". The British Journal of Psychiatry. 204 (5): 335–40. doi:10.1192/bjp.bp.113.131227. PMID 24785767.
^ Lai BS, Lewis R, Livings MS, La Greca AM, Esnard AM (December 2017). "Posttraumatic Stress Symptom Trajectories Among Children After Disaster Exposure: A Review". Journal of Traumatic Stress. 30 (6): 571–582. doi:10.1002/jts.22242. PMC 5953201. PMID 29193316.
^ Koenen KC, Moffitt TE, Poulton R, Martin J, Caspi A (February 2007). "Early childhood factors associated with the development of post-traumatic stress disorder: results from a longitudinal birth cohort". Psychological Medicine. 37 (2): 181–92. doi:10.1017/S0033291706009019. PMC 2254221. PMID 17052377.
^ Lapp KG, Bosworth HB, Strauss JL, Stechuchak KM, Horner RD, Calhoun PS, Meador KG, Lipper S, Butterfield MI (September 2005). "Lifetime sexual and physical victimization among male veterans with combat-related post-traumatic stress disorder". Military Medicine. 170 (9): 787–90. doi:10.7205/MILMED.170.9.787. PMID 16261985.
^ Otte C, Neylan TC, Pole N, Metzler T, Best S, Henn-Haase C, Yehuda R, Marmar CR (January 2005). "Association between childhood trauma and catecholamine response to psychological stress in police academy recruits". Biological Psychiatry. 57 (1): 27–32. doi:10.1016/j.biopsych.2004.10.009. PMID 15607297.
^ Dobry Y, Braquehais MD, Sher L (2013). "Bullying, psychiatric pathology and suicidal behavior". International Journal of Adolescent Medicine and Health. 25 (3): 295–9. doi:10.1515/ijamh-2013-0065. PMID 24006324.
^ abcdefghi Skelton K, Ressler KJ, Norrholm SD, Jovanovic T, Bradley-Davino B (February 2012). "PTSD and gene variants: new pathways and new thinking". Neuropharmacology. 62 (2): 628–37. doi:10.1016/j.neuropharm.2011.02.013. PMC 3136568. PMID 21356219.
^ Laor N, Wolmer L, Mayes LC, Golomb A, Silverberg DS, Weizman R, Cohen DJ (May 1996). "Israeli preschoolers under Scud missile attacks. A developmental perspective on risk-modifying factors". Archives of General Psychiatry. 53 (5): 416–23. doi:10.1001/archpsyc.1996.01830050052008. PMID 8624185.
^ Laor N, Wolmer L, Mayes LC, Gershon A, Weizman R, Cohen DJ (March 1997). "Israeli preschool children under Scuds: a 30-month follow-up". Journal of the American Academy of Child and Adolescent Psychiatry. 36 (3): 349–56. doi:10.1097/00004583-199703000-00013. PMID 9055515. (Subscription required (help)).
^ Janoff-Bulman, R. (1992). Shattered Assumptions: Toward a New Psychology of Trauma. New York: Free Press.
[page needed]
^ abc Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB (December 1995). "Posttraumatic stress disorder in the National Comorbidity Survey". Archives of General Psychiatry. 52 (12): 1048–60. doi:10.1001/archpsyc.1995.03950240066012. PMID 7492257.
^ Liu H, Petukhova MV, Sampson NA, Aguilar-Gaxiola S, Alonso J, Andrade LH, Bromet EJ, de Girolamo G, Haro JM, Hinkov H, Kawakami N, Koenen KC, Kovess-Masfety V, Lee S, Medina-Mora ME, Navarro-Mateu F, O'Neill S, Piazza M, Posada-Villa J, Scott KM, Shahly V, Stein DJ, Ten Have M, Torres Y, Gureje O, Zaslavsky AM, Kessler RC (March 2017). "Association of DSM-IV Posttraumatic Stress Disorder With Traumatic Experience Type and History in the World Health Organization World Mental Health Surveys". JAMA Psychiatry. 74 (3): 270–281. doi:10.1001/jamapsychiatry.2016.3783. PMC 5441566. PMID 28055082.
^ Rothschild, Babette (2000). The Body Remembers: The Psychophysiology of Trauma and Trauma Treatment. New York: W.W. Norton & Company. ISBN 978-0-393-70327-6.
[page needed]
^ Howard LM, Oram S, Galley H, Trevillion K, Feder G (2013). "Domestic violence and perinatal mental disorders: a systematic review and meta-analysis". PLoS Medicine. 10 (5): e1001452. doi:10.1371/journal.pmed.1001452. PMC 3665851. PMID 23723741.
^ Hoffman BL, Schorge JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM, eds. (2016). Williams Gynecology (3rd ed.). McGraw Hill Professional. ISBN 9780071849098.
^ Surís A, Lind L, Kashner TM, Borman PD, Petty F (2004). "Sexual assault in women veterans: an examination of PTSD risk, health care utilization, and cost of care". Psychosomatic Medicine. 66 (5): 749–56. CiteSeerX 10.1.1.508.9827. doi:10.1097/01.psy.0000138117.58559.7b. PMID 15385701.
^ Mason F, Lodrick Z (February 2013). "Psychological consequences of sexual assault". Best Practice & Research. Clinical Obstetrics & Gynaecology. 27 (1): 27–37. doi:10.1016/j.bpobgyn.2012.08.015. PMID 23182852.
^ ab Shalev A, Liberzon I, Marmar C (June 2017). "Post-Traumatic Stress Disorder". The New England Journal of Medicine. 376 (25): 2459–2469. doi:10.1056/NEJMra1612499. PMID 28636846.
^ Hollifield M, Warner TD, Lian N, Krakow B, Jenkins JH, Kesler J, Stevenson J, Westermeyer J (August 2002). "Measuring trauma and health status in refugees: a critical review". JAMA. 288 (5): 611–21. doi:10.1001/jama.288.5.611. PMID 12150673.
^ Porter M, Haslam N (October 2001). "Forced displacement in Yugoslavia: a meta-analysis of psychological consequences and their moderators". Journal of Traumatic Stress. 14 (4): 817–34. doi:10.1023/A:1013054524810. PMID 11776427.
^ ab Atwoli L, Stein DJ, King A, Petukhova M, Aguilar-Gaxiola S, Alonso J, Bromet EJ, de Girolamo G, Demyttenaere K, Florescu S, Maria Haro J, Karam EG, Kawakami N, Lee S, Lepine JP, Navarro-Mateu F, O'Neill S, Pennell BE, Piazza M, Posada-Villa J, Sampson NA, Ten Have M, Zaslavsky AM, Kessler RC (April 2017). "Posttraumatic stress disorder associated with unexpected death of a loved one: Cross-national findings from the world mental health surveys". Depression and Anxiety. 34 (4): 315–326. doi:10.1002/da.22579. PMC 5661943. PMID 27921352.
^ abc "Cancer-Related Post-traumatic Stress". National Cancer Institute. January 1980. Retrieved 2017-09-16.
^ Swartzman S, Booth JN, Munro A, Sani F (April 2017). "Posttraumatic stress disorder after cancer diagnosis in adults: A meta-analysis". Depression and Anxiety (Submitted manuscript). 34 (4): 327–339. doi:10.1002/da.22542. PMID 27466972.
^ Cordova MJ, Riba MB, Spiegel D (April 2017). "Post-traumatic stress disorder and cancer". The Lancet. Psychiatry. 4 (4): 330–338. doi:10.1016/S2215-0366(17)30014-7. PMC 5676567. PMID 28109647.
^ Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y (2012). "Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review". PLOS One. 7 (6): e38915. Bibcode:2012PLoSO...738915E. doi:10.1371/journal.pone.0038915. PMC 3380054. PMID 22745687.
^ Edmondson D, Richardson S, Fausett JK, Falzon L, Howard VJ, Kronish IM (2013-06-19). "Prevalence of PTSD in Survivors of Stroke and Transient Ischemic Attack: A Meta-Analytic Review". PLOS One. 8 (6): e66435. Bibcode:2013PLoSO...866435E. doi:10.1371/journal.pone.0066435. PMC 3686746. PMID 23840467.
^ Abbey G, Thompson SB, Hickish T, Heathcote D (April 2015). "A meta-analysis of prevalence rates and moderating factors for cancer-related post-traumatic stress disorder". Psycho-Oncology. 24 (4): 371–81. doi:10.1002/pon.3654. PMC 4409098. PMID 25146298.
^ Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ (September 2008). "Posttraumatic stress disorder in general intensive care unit survivors: a systematic review". General Hospital Psychiatry. 30 (5): 421–34. doi:10.1016/j.genhosppsych.2008.05.006. PMC 2572638. PMID 18774425.
^ ab Arnaboldi P, Riva S, Crico C, Pravettoni G (2017). "A systematic literature review exploring the prevalence of post-traumatic stress disorder and the role played by stress and traumatic stress in breast cancer diagnosis and trajectory". Breast Cancer. 9: 473–485. doi:10.2147/BCTT.S111101. PMC 5505536. PMID 28740430.
^ ab Liu C, Zhang Y, Jiang H, Wu H (2017-05-05). "Association between social support and post-traumatic stress disorder symptoms among Chinese patients with ovarian cancer: A multiple mediation model". PLOS One. 12 (5): e0177055. Bibcode:2017PLoSO..1277055L. doi:10.1371/journal.pone.0177055. PMC 5419605. PMID 28475593.
^ "PsycNET". psycnet.apa.org. Retrieved 2018-09-30.
^ ab Christiansen DM (February 2017). "Posttraumatic stress disorder in parents following infant death: A systematic review". Clinical Psychology Review. 51: 60–74. doi:10.1016/j.cpr.2016.10.007. PMID 27838460.
^ Kersting A, Wagner B (June 2012). "Complicated grief after perinatal loss". Dialogues in Clinical Neuroscience. 14 (2): 187–94. PMC 3384447. PMID 22754291.
^ Daugirdaitė V, van den Akker O, Purewal S (2015). "Posttraumatic stress and posttraumatic stress disorder after termination of pregnancy and reproductive loss: a systematic review". Journal of Pregnancy. 2015: 646345. doi:10.1155/2015/646345. PMC 4334933. PMID 25734016.
^ Ayers S, Bond R, Bertullies S, Wijma K (April 2016). "The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework". Psychological Medicine. 46 (6): 1121–34. doi:10.1017/s0033291715002706. PMID 26878223.
^ James S (December 2015). "Women's experiences of symptoms of posttraumatic stress disorder (PTSD) after traumatic childbirth: a review and critical appraisal". Archives of Women's Mental Health. 18 (6): 761–71. doi:10.1007/s00737-015-0560-x. PMC 4624822. PMID 26264506.
^ abc Olde E, van der Hart O, Kleber R, van Son M (January 2006). "Posttraumatic stress following childbirth: a review". Clinical Psychology Review. 26 (1): 1–16. doi:10.1016/j.cpr.2005.07.002. hdl:1874/16760. PMID 16176853.
^ Alder J, Stadlmayr W, Tschudin S, Bitzer J (June 2006). "Post-traumatic symptoms after childbirth: what should we offer?". Journal of Psychosomatic Obstetrics and Gynaecology. 27 (2): 107–12. doi:10.1080/01674820600714632. PMID 16808085.
^ Montmasson H, Bertrand P, Perrotin F, El-Hage W (October 2012). "[Predictors of postpartum post-traumatic stress disorder in primiparous mothers]". Journal de Gynecologie, Obstetrique et Biologie de la Reproduction. 41 (6): 553–60. doi:10.1016/j.jgyn.2012.04.010. PMID 22622194.
^ Martin, Colin (2012). Perinatal Mental Health : a Clinical Guide. Cumbria England: M & K Pub. p. 26. ISBN 9781907830495.
^ True WR, Rice J, Eisen SA, Heath AC, Goldberg J, Lyons MJ, Nowak J (April 1993). "A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms". Archives of General Psychiatry. 50 (4): 257–64. doi:10.1001/archpsyc.1993.01820160019002. PMID 8466386.
^ Delahanty DL (January 2011). "Toward the predeployment detection of risk for PTSD". The American Journal of Psychiatry. 168 (1): 9–11. doi:10.1176/appi.ajp.2010.10101519. PMID 21205813.
^ The Secret Life of the Brain (Series), episode 4. PBS. 2001. Archived from the original on 2014-02-02. Retrieved 2014-01-29.
^ ab Zohar J, Juven-Wetzler A, Myers V, Fostick L (January 2008). "Post-traumatic stress disorder: facts and fiction". Current Opinion in Psychiatry. 21 (1): 74–7. doi:10.1097/YCO.0b013e3282f269ee. PMID 18281844.
^ Yehuda R, Halligan SL, Golier JA, Grossman R, Bierer LM (April 2004). "Effects of trauma exposure on the cortisol response to dexamethasone administration in PTSD and major depressive disorder". Psychoneuroendocrinology. 29 (3): 389–404. doi:10.1016/S0306-4530(03)00052-0. PMID 14644068.
^ Yehuda R, Halligan SL, Grossman R, Golier JA, Wong C (September 2002). "The cortisol and glucocorticoid receptor response to low dose dexamethasone administration in aging combat veterans and holocaust survivors with and without posttraumatic stress disorder". Biological Psychiatry. 52 (5): 393–403. doi:10.1016/S0006-3223(02)01357-4. PMID 12242055.
^ Heim C, Ehlert U, Hellhammer DH (January 2000). "The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders". Psychoneuroendocrinology. 25 (1): 1–35. doi:10.1016/S0306-4530(99)00035-9. PMID 10633533.
^ Mason JW, Giller EL, Kosten TR, Harkness L (August 1988). "Elevation of urinary norepinephrine/cortisol ratio in posttraumatic stress disorder". The Journal of Nervous and Mental Disease. 176 (8): 498–502. doi:10.1097/00005053-198808000-00008. PMID 3404142.
^ Bohnen N, Nicolson N, Sulon J, Jolles J (1991). "Coping style, trait anxiety and cortisol reactivity during mental stress". Journal of Psychosomatic Research. 35 (2–3): 141–7. CiteSeerX 10.1.1.467.4323. doi:10.1016/0022-3999(91)90068-Y. PMID 2046048.
^ Geracioti TD, Baker DG, Ekhator NN, West SA, Hill KK, Bruce AB, Schmidt D, Rounds-Kugler B, Yehuda R, Keck PE, Kasckow JW (August 2001). "CSF norepinephrine concentrations in posttraumatic stress disorder". The American Journal of Psychiatry. 158 (8): 1227–30. doi:10.1176/appi.ajp.158.8.1227. PMID 11481155.
^ Sautter FJ, Bissette G, Wiley J, Manguno-Mire G, Schoenbachler B, Myers L, Johnson JE, Cerbone A, Malaspina D (December 2003). "Corticotropin-releasing factor in posttraumatic stress disorder (PTSD) with secondary psychotic symptoms, nonpsychotic PTSD, and healthy control subjects". Biological Psychiatry. 54 (12): 1382–8. doi:10.1016/S0006-3223(03)00571-7. PMID 14675802.
^ de Kloet CS, Vermetten E, Geuze E, Lentjes EG, Heijnen CJ, Stalla GK, Westenberg HG (2008). "Elevated plasma corticotrophin-releasing hormone levels in veterans with posttraumatic stress disorder". Stress Hormones and Post Traumatic Stress Disorder Basic Studies and Clinical Perspectives. Progress in Brain Research. 167. pp. 287–91. doi:10.1016/S0079-6123(07)67025-3. ISBN 978-0-444-53140-7. PMID 18037027.
^ Radley JJ, Kabbaj M, Jacobson L, Heydendael W, Yehuda R, Herman JP (September 2011). "Stress risk factors and stress-related pathology: neuroplasticity, epigenetics and endophenotypes". Stress. 14 (5): 481–97. doi:10.3109/10253890.2011.604751. PMC 3641164. PMID 21848436.
^ Pitman RK (July 1989). "Post-traumatic stress disorder, hormones, and memory". Biological Psychiatry. 26 (3): 221–3. doi:10.1016/0006-3223(89)90033-4. PMID 2545287.
^ Yehuda R (2001). "Biology of posttraumatic stress disorder". The Journal of Clinical Psychiatry. 62. 62 Suppl 17: 41–6. PMID 11495096.
^ Yehuda R (2002). "Clinical relevance of biologic findings in PTSD". The Psychiatric Quarterly. 73 (2): 123–33. doi:10.1023/A:1015055711424. PMID 12025720.
^ Aardal-Eriksson E, Eriksson TE, Thorell LH (December 2001). "Salivary cortisol, posttraumatic stress symptoms, and general health in the acute phase and during 9-month follow-up". Biological Psychiatry. 50 (12): 986–93. doi:10.1016/S0006-3223(01)01253-7. PMID 11750895.
^ abcde Olszewski TM, Varrasse JF (June 2005). "The neurobiology of PTSD: implications for nurses". Journal of Psychosocial Nursing and Mental Health Services. 43 (6): 40–7. PMID 16018133.
^ Chatzitomaris A, Hoermann R, Midgley JE, Hering S, Urban A, Dietrich B, Abood A, Klein HH, Dietrich JW (20 July 2017). "Thyroid Allostasis-Adaptive Responses of Thyrotropic Feedback Control to Conditions of Strain, Stress, and Developmental Programming". Frontiers in Endocrinology. 8: 163. doi:10.3389/fendo.2017.00163. PMC 5517413. PMID 28775711.
^ Lindley SE, Carlson EB, Benoit M (May 2004). "Basal and dexamethasone suppressed salivary cortisol concentrations in a community sample of patients with posttraumatic stress disorder". Biological Psychiatry. 55 (9): 940–5. doi:10.1016/j.biopsych.2003.12.021. PMID 15110738.
^ "NIMH · Post Traumatic Stress Disorder Research Fact Sheet". National Institutes of Health. Archived from the original on 2014-01-23. Retrieved 2014-01-29.
^ Bromis K, Calem M, Reinders AA, Williams SC, Kempton MJ (July 2018). "Meta-Analysis of 89 Structural MRI Studies in Posttraumatic Stress Disorder and Comparison With Major Depressive Disorder". The American Journal of Psychiatry. 175 (10): 989–998. doi:10.1176/appi.ajp.2018.17111199. PMC 6169727. PMID 30021460.
^ Liberzon I, Sripada CS (2008). "The functional neuroanatomy of PTSD: A critical review". Stress Hormones and Post Traumatic Stress Disorder Basic Studies and Clinical Perspectives. Progress in Brain Research. 167. pp. 151–69. doi:10.1016/S0079-6123(07)67011-3. ISBN 9780444531407. PMID 18037013.
^ Hughes KC, Shin LM (February 2011). "Functional neuroimaging studies of post-traumatic stress disorder". Expert Review of Neurotherapeutics. 11 (2): 275–85. doi:10.1586/ern.10.198. PMC 3142267. PMID 21306214.
^ Etkin A, Wager TD (October 2007). "Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia". The American Journal of Psychiatry. 164 (10): 1476–88. doi:10.1176/appi.ajp.2007.07030504. PMC 3318959. PMID 17898336.
^ van der Kolk B (March 2000). "Posttraumatic stress disorder and the nature of trauma". Dialogues in Clinical Neuroscience. 2 (1): 7–22. PMC 3181584. PMID 22034447.
^ ab Milad MR, Pitman RK, Ellis CB, Gold AL, Shin LM, Lasko NB, Zeidan MA, Handwerger K, Orr SP, Rauch SL (December 2009). "Neurobiological basis of failure to recall extinction memory in posttraumatic stress disorder". Biological Psychiatry. 66 (12): 1075–82. doi:10.1016/j.biopsych.2009.06.026. PMC 2787650. PMID 19748076.
^ Stein MB, Paulus MP (December 2009). "Imbalance of approach and avoidance: the yin and yang of anxiety disorders". Biological Psychiatry. 66 (12): 1072–4. doi:10.1016/j.biopsych.2009.09.023. PMC 2825567. PMID 19944792.
^ Goodkind M, Etkin A. "Functional Neurocircuitry and Neuroimaging Studies of Anxiety Disorders". In Sklar P, Buxbaum J, Nestler E, Charney D. Neurobiology of Mental Illness (5th ed.). Oxford University Press.
^ Carlson, Neil R. (2007). Physiology of Behavior (9 ed.). Pearson Education, Inc.[full citation needed]
^ Jatzko A, Rothenhöfer S, Schmitt A, Gaser C, Demirakca T, Weber-Fahr W, Wessa M, Magnotta V, Braus DF (August 2006). "Hippocampal volume in chronic posttraumatic stress disorder (PTSD): MRI study using two different evaluation methods" (PDF). Journal of Affective Disorders. 94 (1–3): 121–6. doi:10.1016/j.jad.2006.03.010. PMID 16701903. Archived (PDF) from the original on 2013-10-19.
^ First MB (2013). DSM-5® Handbook of Differential Diagnosis. American Psychiatric Pub. p. 225. ISBN 9781585629985.
^ "Trauma- and Stressor-Related Disorders", Diagnostic and Statistical Manual of Mental Disorders, American Psychiatric Association, 2013-05-22, doi:10.1176/appi.books.9780890425596.dsm07, ISBN 978-0890425558
^ "PTSD Checklist for DSM-5 (PCL-5)". National Center for PTSD. 11 May 2017.
^ Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL (December 2015). "The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation". Journal of Traumatic Stress. 28 (6): 489–98. doi:10.1002/jts.22059. PMID 26606250.
^ "Primary Care PTSD Screen for DSM-5 (PC-PTSD-5)". National Center for PTSD. 7 Apr 2017.
^ "Child PTSD Symptom Scale". International Society for Traumatic Stress Studies.
^ Foa EB, Johnson KM, Feeny NC, Treadwell KR (September 2001). "The child PTSD Symptom Scale: a preliminary examination of its psychometric properties". Journal of Clinical Child Psychology. 30 (3): 376–84. doi:10.1207/S15374424JCCP3003_9. PMID 11501254.
^ "Child Trauma Screening Questionnaire". The National Child Traumatic Stress Network. 5 Sep 2013.
^ Kenardy JA, Spence SH, Macleod AC (September 2006). "Screening for posttraumatic stress disorder in children after accidental injury". Pediatrics. 118 (3): 1002–9. doi:10.1542/peds.2006-0406. PMID 16950991.
^ "UCLA Posttraumatic Stress Disorder Reaction Index". International Society for Traumatic Stress Studies.
^ Elhai JD, Layne CM, Steinberg AM, Brymer MJ, Briggs EC, Ostrowski SA, Pynoos RS (February 2013). "Psychometric properties of the UCLA PTSD reaction index. part II: investigating factor structure findings in a national clinic-referred youth sample". Journal of Traumatic Stress. 26 (1): 10–8. doi:10.1002/jts.21755. PMID 23417874.
^ ab Scheeringa M. "Young Child PTSD Screen". Tulane University. Retrieved 8 April 2018.
^ Scheeringa MS, Haslett N (June 2010). "The reliability and criterion validity of the Diagnostic Infant and Preschool Assessment: a new diagnostic instrument for young children". Child Psychiatry and Human Development. 41 (3): 299–312. doi:10.1007/s10578-009-0169-2. PMC 2862973. PMID 20052532.
^ ab "The ICD-10 Classification of Mental and Behavioural Disorders" (PDF). World Health Organization. pp. 120–121. Archived (PDF) from the original on 2014-03-23. Retrieved 2014-01-29.
^ "WHO releases new International Classification of Diseases (ICD 11)". World Health Organization. Retrieved 2018-11-15.
^ abcd Brewin, Chris R.; Cloitre, Marylène; Hyland, Philip; Shevlin, Mark; Maercker, Andreas; Bryant, Richard A.; Humayun, Asma; Jones, Lynne M.; Kagee, Ashraf (2017). "A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD". Clinical Psychology Review. 58: 1–15. doi:10.1016/j.cpr.2017.09.001. ISSN 1873-7811. PMID 29029837.
^ Herman JL (July 1992). "Complex PTSD: A syndrome in survivors of prolonged and repeated trauma". Journal of Traumatic Stress. 5 (3): 377–391. doi:10.1007/BF00977235.
^ Herman JL (1997). Trauma and Recovery (2nd ed.). New York: Basic Books. pp. 119–122. ISBN 978-0-465-08730-3.
^ Carlier IV, Lamberts RD, van Uchelen AJ, Gersons BP (1998). "Disaster-related post-traumatic stress in police officers: A field study of the impact of debriefing". Stress Medicine. 14 (3): 143–8. doi:10.1002/(SICI)1099-1700(199807)14:3<143::AID-SMI770>3.0.CO;2-S.
^ Mayou RA, Ehlers A, Hobbs M (June 2000). "Psychological debriefing for road traffic accident victims. Three-year follow-up of a randomised controlled trial". The British Journal of Psychiatry. 176 (6): 589–93. doi:10.1192/bjp.176.6.589. PMID 10974967.
^ ab Roberts NP, Kitchiner NJ, Kenardy J, Bisson J (July 2009). "Multiple session early psychological interventions for the prevention of post-traumatic stress disorder". The Cochrane Database of Systematic Reviews (3): CD006869. doi:10.1002/14651858.CD006869.pub2. PMID 19588408.
^ Assessment and Management of Conditions Specifically Related to Stress (PDF). Geneva: World Health Organization. 2013. ISBN 978-92-4-150593-2. Archived (PDF) from the original on 2014-02-01. Retrieved 2014-01-29.
^ Amos T, Stein DJ, Ipser JC (July 2014). "Pharmacological interventions for preventing post-traumatic stress disorder (PTSD)". The Cochrane Database of Systematic Reviews. 7 (7): CD006239. doi:10.1002/14651858.CD006239.pub2. PMID 25001071.
^ ab Gartlehner G, Forneris CA, Brownley KA, Gaynes BN, Sonis J, Coker-Schwimmer E, Jonas DE, Greenblatt A, Wilkins TM, Woodell CL, Lohr KN (2013). Interventions for the Prevention of Posttraumatic Stress Disorder (PTSD) in Adults After Exposure to Psychological Trauma. Agency for Healthcare Research and Quality (US). PMID 23658936.
^ Feldner MT, Monson CM, Friedman MJ (January 2007). "A critical analysis of approaches to targeted PTSD prevention: current status and theoretically derived future directions". Behavior Modification. 31 (1): 80–116. CiteSeerX 10.1.1.595.9186. doi:10.1177/0145445506295057. PMID 17179532.
^ Rose S, Bisson J, Churchill R, Wessely S (2002). "Psychological debriefing for preventing post traumatic stress disorder (PTSD)". The Cochrane Database of Systematic Reviews (2): CD000560. doi:10.1002/14651858.CD000560. PMID 12076399.
^ "Psychological Debriefing for Post-Traumatic Stress Disorder". www.div12.org. Society of Clinical Psychology: Division 12 of The American Psychological Association. Retrieved 9 September 2017.
^ Wiseman T, Foster K, Curtis K (November 2013). "Mental health following traumatic physical injury: an integrative literature review". Injury. 44 (11): 1383–90. doi:10.1016/j.injury.2012.02.015. PMID 22409991.
^ Kassam-Adams N, Marsac ML, Hildenbrand A, Winston F (December 2013). "Posttraumatic stress following pediatric injury: update on diagnosis, risk factors, and intervention". JAMA Pediatrics. 167 (12): 1158–65. doi:10.1001/jamapediatrics.2013.2741. PMID 24100470.
^ Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB (August 2010). "A meta-analytic review of prolonged exposure for posttraumatic stress disorder". Clinical Psychology Review. 30 (6): 635–41. doi:10.1016/j.cpr.2010.04.007. PMID 20546985.
^ Guideline Development Panel for the Treatment of PTSD in Adults (2017). Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults (PDF). Washington, D.C.: American Psychological Association. pp. ES–2.
^ ab Lee CW, Cuijpers P (June 2013). "A meta-analysis of the contribution of eye movements in processing emotional memories". Journal of Behavior Therapy and Experimental Psychiatry (Submitted manuscript). 44 (2): 231–9. doi:10.1016/j.jbtep.2012.11.001. PMID 23266601.
^ Cahill SP, Foa EB (2004). Taylor S, ed. Advances in the Treatment of Posttraumatic Stress Disorder: Cognitive-behavioral perspectives. New York: Springer. pp. 267–313.
^ VA/DOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder (PDF). United States Department of Veterans Affairs. 2017. pp. 46–47.
^ Seidler GH, Wagner FE (November 2006). "Comparing the efficacy of EMDR and trauma-focused cognitive-behavioral therapy in the treatment of PTSD: a meta-analytic study". Psychological Medicine. 36 (11): 1515–22. doi:10.1017/S0033291706007963. PMID 16740177.
^ ab Moreno-Alcázar A, Treen D, Valiente-Gómez A, Sio-Eroles A, Pérez V, Amann BL, Radua J (2017). "Efficacy of Eye Movement Desensitization and Reprocessing in Children and Adolescent with Post-traumatic Stress Disorder: A Meta-Analysis of Randomized Controlled Trials". Frontiers in Psychology. 8: 1750. doi:10.3389/fpsyg.2017.01750. PMC 5641384. PMID 29066991.
^ Rolfsnes ES, Idsoe T (April 2011). "School-based intervention programs for PTSD symptoms: a review and meta-analysis". Journal of Traumatic Stress. 24 (2): 155–65. doi:10.1002/jts.20622. PMID 21425191.
^ "Treatment of PTSD – PTSD: National Center for PTSD". U.S. Department of Veterans Affairs. May 26, 2016. Archived from the original on December 1, 2016.
^ "PTSD Treatment Options". Defense Centers of Excellence. November 23, 2016. Archived from the original on November 30, 2016.
^ "Cognitive Behavioral Therapy (CBT) for Treatment of PTSD". www.apa.org. Archived from the original on 2018-01-09. Retrieved 2018-01-08.
^ "Treatment of PTSD - PTSD: National Center for PTSD". www.ptsd.va.gov. Retrieved 2018-01-08.
^ Mulick PS, Landes S, Kanter JW (2005). "Contextual Behavior Therapies in the Treatment of PTSD: A Review" (PDF). International Journal of Behavioral Consultation and Therapy. 1 (3): 223–228. CiteSeerX 10.1.1.625.4407. doi:10.1037/h0100747.
^ Hassija CM, Gray MJ (2007). "Behavioral Interventions for Trauma and Posttraumatic Stress Disorder". International Journal of Behavioral Consultation and Therapy. 3 (2): 166–175. doi:10.1037/h0100797.
^ Mulick PS, Naugle AE (2009). "Behavioral Activation in the Treatment of Comorbid Posttraumatic Stress Disorder and Major Depressive Disorder". International Journal of Behavioral Consultation and Therapy. 5 (2): 330–339. doi:10.1037/h0100892.
^ Grohol, JM (2016-05-17). "What is Exposure Therapy?". Psychcentral.com. Archived from the original on 2010-08-11. Retrieved 2010-07-14.
^ Joseph JS, Gray MJ (2008). "Exposure Therapy for Posttraumatic Stress Disorder" (PDF). Journal of Behavior Analysis of Offender and Victim: Treatment and Prevention. 1 (4): 69–80. doi:10.1037/h0100457. Archived from the original (PDF) on 2010-12-29. Retrieved 2010-05-10.
^ Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, Pynoos JD, Zatzick DF, Benedek DM, McIntyre JS, Charles SC, Altshuler K, Cook I, Cross CD, Mellman L, Moench LA, Norquist G, Twemlow SW, Woods S, Yager J (November 2004). "Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder". The American Journal of Psychiatry. 161 (11 Suppl): 3–31. PMID 15617511.
^ Committee on Treatment of Posttraumatic Stress Disorder, Institute of Medicine: Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, D.C.: National Academies Press. 2008. ISBN 978-0-309-10926-0.
[page needed]
^ "Prolonged Exposure Therapy". U.S. Department of Veteran Affairs. PTSD: National Center for PTSD. 2009-09-29. Archived from the original on 2009-11-14. Retrieved 2010-07-14.
^ Karlin BE, Ruzek JI, Chard KM, Eftekhari A, Monson CM, Hembree EA, Resick PA, Foa EB (December 2010). "Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration". Journal of Traumatic Stress. 23 (6): 663–73. doi:10.1002/jts.20588. PMID 21171126.
^ ab Shapiro F (April 1989). "Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories". Journal of Traumatic Stress. 2 (2): 199–223. doi:10.1002/jts.2490020207.
^ Shapiro F, Maxfield L (August 2002). "Eye Movement Desensitization and Reprocessing (EMDR): information processing in the treatment of trauma". Journal of Clinical Psychology. 58 (8): 933–46. doi:10.1002/jclp.10068. PMID 12115716.
^ ab The Management of Post-Traumatic Stress Working Group (2010). "VA/DoD clinical practice guideline for management of post-traumatic stress". Department of Veterans Affairs, Department of Defense. p. Version 2.0. Archived from the original on 30 May 2013. Retrieved 2 June 2013.
^ abc Gillies D, Taylor F, Gray C, O'Brien L, D'Abrew N (December 2012). "Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents". The Cochrane Database of Systematic Reviews. 12: CD006726. doi:10.1002/14651858.CD006726.pub2. PMID 23235632.
^ ab Jeffries FW, Davis P (May 2013). "What is the role of eye movements in eye movement desensitization and reprocessing (EMDR) for post-traumatic stress disorder (PTSD)? a review". Behavioural and Cognitive Psychotherapy. 41 (3): 290–300. doi:10.1017/S1352465812000793. PMID 23102050.
^ abcdef Jonas DE, Cusack K, Forneris CA (April 2013). "Psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD)". Comparative Effectiveness Reviews (92). Rockville, MD: US Agency for Healthcare Quality and Research. PMID 23658937. Archived from the original on 2013-10-01. Lay summary – Pubmed Health (plain English).

^ Brewin CR, Andrews B, Valentine JD (October 2000). "Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults". Journal of Consulting and Clinical Psychology. 68 (5): 748–66. doi:10.1037/0022-006X.68.5.748. PMID 11068961.
^ Ozer EJ, Best SR, Lipsey TL, Weiss DS (January 2003). "Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis". Psychological Bulletin. 129 (1): 52–73. doi:10.1037/0033-2909.129.1.52. PMID 12555794.
^ Weissman MM, Markowitz JC, Klerman GL (2007). Clinician's Quick Guide to Interpersonal Psychotherapy. New York: Oxford University Press.
[page needed]
^ Bleiberg KL, Markowitz JC (January 2005). "A pilot study of interpersonal psychotherapy for posttraumatic stress disorder". The American Journal of Psychiatry. 162 (1): 181–3. doi:10.1176/appi.ajp.162.1.181. PMID 15625219.
^ "Trauma and PTSD Program – Columbia University Department of Psychiatry". Columbiatrauma.org. Archived from the original on 2014-02-01. Retrieved 2014-01-29.
[full citation needed]
^ Markowitz JC, Milrod B, Bleiberg K, Marshall RD (March 2009). "Interpersonal factors in understanding and treating posttraumatic stress disorder". Journal of Psychiatric Practice. 15 (2): 133–40. doi:10.1097/01.pra.0000348366.34419.28. PMC 2852131. PMID 19339847.
^ Markowitz JC (October 2010). "IPT and PTSD". Depression and Anxiety. 27 (10): 879–81. doi:10.1002/da.20752. PMC 3683871. PMID 20886608.
^ Krystal JH, Neumeister A (October 2009). "Noradrenergic and serotonergic mechanisms in the neurobiology of posttraumatic stress disorder and resilience". Brain Research. 1293: 13–23. doi:10.1016/j.brainres.2009.03.044. PMC 2761677. PMID 19332037.
^ ab Jeffreys M, Capehart B, Friedman MJ (2012). "Pharmacotherapy for posttraumatic stress disorder: review with clinical applications" (PDF). Journal of Rehabilitation Research and Development. 49 (5): 703–15. doi:10.1682/JRRD.2011.09.0183. PMID 23015581. Archived (PDF) from the original on 4 March 2016.While evidence-based, trauma-focused psychotherapy is the preferred treatment for PTSD, pharmacotherapy is also an important treatment option. First-line pharmacotherapy agents include selective serotonin reuptake inhibitors and the selective serotonin-norepinephrine reuptake inhibitor venlafaxine.
^ Puetz TW, Youngstedt SD, Herring MP (28 May 2015). Hashimoto K, ed. "Effects of Pharmacotherapy on Combat-Related PTSD, Anxiety, and Depression: A Systematic Review and Meta-Regression Analysis". PLOS One. 10 (5): e0126529. Bibcode:2015PLoSO..1026529P. doi:10.1371/journal.pone.0126529. PMC 4447407. PMID 26020791.The cumulative evidence summarized in this review indicates that pharmacotherapy significantly reduces PTSD, anxiety, and depressive symptom severity among combat veterans with PTSD. The magnitude of the overall effects of pharmacotherapy on PTSD (Δ = 0.38), anxiety (Δ = 0.42), and depressive symptoms (Δ = 0.52) were moderate...
^ Kapfhammer HP (June 2014). "Patient-reported outcomes in post-traumatic stress disorder. Part II: focus on pharmacological treatment". Dialogues in Clinical Neuroscience (in English, Spanish, and French). 16 (2): 227–37. PMC 4140515. PMID 25152660.
^ Jain S, Greenbaum MA, Rosen C (February 2012). "Concordance between psychotropic prescribing for veterans with PTSD and clinical practice guidelines". Psychiatric Services. 63 (2): 154–60. doi:10.1176/appi.ps.201100199. PMID 22302333.
^ Auxéméry Y (October 2012). "[Posttraumatic stress disorder (PTSD) as a consequence of the interaction between an individual genetic susceptibility, a traumatogenic event and a social context]". L'Encephale (in French). 38 (5): 373–80. doi:10.1016/j.encep.2011.12.003. PMID 23062450.
^ Kapfhammer HP (December 2008). "[Therapeutic possibilities after traumatic experiences]". Psychiatria Danubina. 20 (4): 532–45. PMID 19011595.
^ Reist, C (2005). Post-traumatic Stress Disorder. Compendia, Build ID: F000005, published by Epocrates.com
^ Maxmen JS, Ward NG (2002). Psychotropic drugs: fast facts (3rd ed.). New York: W. W. Norton. p. 349. ISBN 978-0-393-70301-6.
^ Martényi F (March 2005). "[Three paradigms in the treatment of posttraumatic stress disorder]". Neuropsychopharmacologia Hungarica. 7 (1): 11–21. PMID 16167463.
^ ab Veterans Affairs and Department of Defense clinical practice guideline for management of post-traumatic stress. VA/DoD. 2010.
^ Bandelow B, Zohar J, Hollander E, Kasper S, Möller HJ, Zohar J, Hollander E, Kasper S, Möller HJ, Bandelow B, Allgulander C, Ayuso-Gutierrez J, Baldwin DS, Buenvicius R, Cassano G, Fineberg N, Gabriels L, Hindmarch I, Kaiya H, Klein DF, Lader M, Lecrubier Y, Lépine JP, Liebowitz MR, Lopez-Ibor JJ, Marazziti D, Miguel EC, Oh KS, Preter M, Rupprecht R, Sato M, Starcevic V, Stein DJ, van Ameringen M, Vega J (2008). "World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders - first revision". The World Journal of Biological Psychiatry. 9 (4): 248–312. doi:10.1080/15622970802465807. PMID 18949648.
^ Griffin GD, Charron D, Al-Daccak R (November 2014). "Post-traumatic stress disorder: revisiting adrenergics, glucocorticoids, immune system effects and homeostasis". Clinical & Translational Immunology. 3 (11): e27. doi:10.1038/cti.2014.26. PMC 4255796. PMID 25505957.
^ O'Neil ME, Nugent SM, Morasco BJ, Freeman M, Low A, Kondo K, Zakher B, Elven C, Motu'apuaka M, Paynter R, Kansagara D (September 2017). "Benefits and Harms of Plant-Based Cannabis for Posttraumatic Stress Disorder: A Systematic Review". Annals of Internal Medicine. 167 (5): 332–340. doi:10.7326/M17-0477. PMID 28806794.
^ Betthauser K, Pilz J, Vollmer LE (August 2015). "Use and effects of cannabinoids in military veterans with posttraumatic stress disorder". American Journal of Health-System Pharmacy (Review). 72 (15): 1279–84. doi:10.2146/ajhp140523. PMID 26195653.
^ "Long-term Nabilone Use: A Review of the Clinical Effectiveness and Safety". CADTH Rapid Response Reports. Oct 2015. PMID 26561692.
^ Gregg K (2016-07-13). "Raimondo signs law allowing marijuana for treatment of PTSD". Providence Journal. Archived from the original on 16 August 2016. Retrieved 18 August 2016.
^ Lawrence S, De Silva M, Henley R (January 2010). Lawrence S, ed. "Sports and games for post-traumatic stress disorder (PTSD)". The Cochrane Database of Systematic Reviews (1): CD007171. doi:10.1002/14651858.CD007171.pub2. PMID 20091620. Archived from the original on 2014-02-01.
^ Jankowski, K. "PTSD and physical health". Information on trauma and PTSD for professionals, National Center for PTSD. U.S. Department of Veterans Affairs. Archived from the original on 30 July 2009. Retrieved 8 June 2013.
^ U.S. Department of Veterans Affairs. "Lifestyle Changes Recommended for PTSD Patients". Information on trauma and PTSD for veterans, general public and family from the National Center for PTSD. U.S. Department of Veterans Affairs. Archived from the original on 31 July 2009. Retrieved 8 June 2013.
^ ab Wethington HR, Hahn RA, Fuqua-Whitley DS, Sipe TA, Crosby AE, Johnson RL, Liberman AM, Mościcki E, Price LN, Tuma FK, Kalra G, Chattopadhyay SK (September 2008). "The effectiveness of interventions to reduce psychological harm from traumatic events among children and adolescents: a systematic review". American Journal of Preventive Medicine. 35 (3): 287–313. doi:10.1016/j.amepre.2008.06.024. PMID 18692745. Archived from the original on 3 February 2014.
^ Fletcher KE, Barkley RA (2003). "7". In Mash EJ. Child psychopathology (2nd ed.). New York: Guilford Press. pp. 330–371. ISBN 978-1-57230-609-7.
^ "Marine Corps Offers Yoga, Massages to Marriages Strained by War". Fox News Channel. Associated Press. 2008-04-02. Archived from the original on 2008-04-05. Retrieved 2008-04-03.
^ Sweeney, Heather (November 6, 2015). "Private Hospital Network to Help VA with Mental Health Care for Vets". Military.com. Archived from the original on March 30, 2017. Retrieved 2017-03-29.
^ Cullen, Kevin (May 2, 2016). "Covering all the bases for veterans". Boston Globe. Archived from the original on March 30, 2017. Retrieved 2017-03-29.
^ "Mortality and Burden of Disease Estimates for WHO Member States in 2004". World Health Organization.
^ Brunet A, Akerib V, Birmes P (August 2007). "Don't throw out the baby with the bathwater (PTSD is not overdiagnosed)". Canadian Journal of Psychiatry. 52 (8): 501–2, discussion 503. doi:10.1177/070674370705200805. PMID 17955912. Archived from the original (PDF) on 2008-12-02.
^ Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ (October 2013). "National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria". Journal of Traumatic Stress. 26 (5): 537–47. doi:10.1002/jts.21848. PMC 4096796. PMID 24151000.
^ ab "Mortality and Burden of Disease Estimates for WHO Member States: Persons, all ages (2004)" (xls). World Health Organization. 2004. Retrieved 2009-11-12.
^ ab "Mortality and Burden of Disease Estimates for WHO Member States: Females, all ages (2004)" (xls). World Health Organization. 2004. Retrieved 2009-11-12.
^ ab "Mortality and Burden of Disease Estimates for WHO Member States: Males, all ages (2004)" (xls). World Health Organization. 2004. Retrieved 2009-11-12.
^ ab Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, Karam EG, Meron Ruscio A, Benjet C, Scott K, Atwoli L, Petukhova M, Lim CC, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Bunting B, Ciutan M, de Girolamo G, Degenhardt L, Gureje O, Haro JM, Huang Y, Kawakami N, Lee S, Navarro-Mateu F, Pennell BE, Piazza M, Sampson N, Ten Have M, Torres Y, Viana MC, Williams D, Xavier M, Kessler RC (October 2017). "Posttraumatic stress disorder in the World Mental Health Surveys". Psychological Medicine. 47 (13): 2260–2274. doi:10.1017/S0033291717000708. PMC 6034513. PMID 28385165.
^ Sher L (August 2010). "Neurobiology of suicidal behavior in post-traumatic stress disorder". Expert Review of Neurotherapeutics. 10 (8): 1233–5. doi:10.1586/ern.10.114. PMID 20662745.
^ Mintz, S. (2007). "The War's Costs". Digital History. Archived from the original on 2003-09-07.
^ Price, Jennifer L. "Findings from the National Vietnam Veterans' Readjustment Study – Factsheet". United States Department of Veterans Affairs. National Center for PTSD. Archived from the original on 2009-04-30.
^ "Psychological Costs of War: Military Combat and Mental Health". Journalistsresource.org. 2012-02-27. Archived from the original on 2014-02-02. Retrieved 2014-01-29.
^ Spoont, M.; Arbisi, P.; Fu, S.; Greer, N.; Kehle-Forbes, S.; Meis, L.; Rutks, I.; Wilt, T. J. (January 2013). "Screening for Post-Traumatic Stress Disorder (PTSD) in Primary Care: A Systematic Review". VA Evidence-based Synthesis Program Reports. Department of Veterans Affairs. PMID 23487872. Lay summary – Pubmed Health (plain English).

^ Meade BJ, Glenn MK, Wirth O (March 29, 2013). "Mission Critical: Getting Vets With PTSD Back to Work". NIOSH: Workplace Safety and Health. Medscape & NIOSH. Archived from the original on March 16, 2016.
^ abcdef Lowell A, Suarez-Jimenez B, Helpman L, Zhu X, Durosky A, Hilburn A, Schneier F, Gross R, Neria Y (March 2018). "9/11-related PTSD among highly exposed populations: a systematic review 15 years after the attack". Psychological Medicine. 48 (4): 537–553. doi:10.1017/S0033291717002033. PMC 5805615. PMID 28805168.
^ abcd Perrin MA, DiGrande L, Wheeler K, Thorpe L, Farfel M, Brackbill R (September 2007). "Differences in PTSD prevalence and associated risk factors among World Trade Center disaster rescue and recovery workers". The American Journal of Psychiatry. 164 (9): 1385–94. doi:10.1176/appi.ajp.2007.06101645. PMID 17728424.
^ abcde Stellman JM, Smith RP, Katz CL, Sharma V, Charney DS, Herbert R, Moline J, Luft BJ, Markowitz S, Udasin I, Harrison D, Baron S, Landrigan PJ, Levin SM, Southwick S (September 2008). "Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster". Environmental Health Perspectives. 116 (9): 1248–53. doi:10.1289/ehp.11164. PMC 2535630. PMID 18795171.
^ "VA Compensation Rate Table". Department of Veterans Affairs. Archived from the original on 3 November 2012. Retrieved 20 October 2012.
^ "Access VA Health Benefits". Department of Veterans Affairs. Archived from the original on 16 October 2012. Retrieved 20 October 2012.
^ "VA Vocational Rehabilitation". Department of Veterans Affairs. Archived from the original on 19 October 2012. Retrieved 20 October 2012.
^ "Vet Success". Department of Veterans Affairs + State Government Veterans Agencies. Archived from the original on 19 October 2012. Retrieved 20 October 2012.
^ "Independent Living Support for Veterans". Department of Veterans Affairs. Archived from the original on 24 October 2012. Retrieved 20 October 2012.
^ "Veterans Benefits". Veterans Benefits Administration. Archived from the original on 26 November 2012. Retrieved 30 November 2012.
^ Dixon, Laura (February 28, 2009). "Lance Corporal Johnson Beharry accuses Government of neglecting soldiers". The Times. London. Retrieved 2009-08-29.
(subscription required)
^ "UK | Full interview: L/Cpl Johnson Beharry". BBC News. 2009-02-28. Archived from the original on 2014-02-19. Retrieved 2009-08-29.
^ "The Operational Stress Injury Social Support (OSISS) Program for Canadian Veterans". Archived from the original on 6 July 2011. See also "Evaluation of the OSISS Peer Support Network" (PDF). Dept. of National Defence and Veterans Affairs Canada. January 2005. Archived (PDF) from the original on 2014-01-30.
^ Heber A, Grenier S, Richardson D, Darte K (2006). "Combining Clinical Treatment and Peer Support: A Unique Approach to Overcoming Stigma and Delivering Care" (PDF). Human Dimensions in Military Operations – Military Leaders’ Strategies for Addressing Stress and Psychological Support. Neuilly-sur-Seine, France: Canadian Department Of National Defence. Archived from the original on 2012-10-07. Retrieved 2014-01-30.
^ Richardson JD, Darte K, Grenier S, English A, Sharpe J (2008). "Operational Stress Injury Social Support: a Canadian innovation in professional peer support". Canadian Military Journal. 9 (1): 57–64. Archived from the original on 2013-12-21. Retrieved 2014-01-30.
^ "The New Veterans Charter for CF Veterans and their Families". Vac-Acc.Gc.Ca. 2006-07-12. Archived from the original on 2006-06-19. Retrieved 2009-08-29.
^ ab Andreasen NC (October 2010). "Posttraumatic stress disorder: a history and a critique". Annals of the New York Academy of Sciences. 1208 (Psychiatric and Neurologic Aspects of War): 67–71. Bibcode:2010NYASA1208...67A. doi:10.1111/j.1749-6632.2010.05699.x. PMID 20955327.
^ ab American Psychiatric Association (1952). Diagnostic and Statistical Manual. American Psychiatric Association Mental Hospital Service. p. 326.3. ISBN 978-0890420171.
^ ab Shalev AY, Yehuda R, McFarlane AC (2000). International handbook of human response to trauma. New York: Kluwer Academic/Plenum Press. ISBN 978-0-306-46095-1.
[page needed];on-line.
^ "International Statistical Classification of Diseases and Related Health Problems 10th Revision Version for 2007". World Health Organization (UN). 2007. Archived from the original on December 5, 2014. Retrieved October 3, 2011.
^ "When trauma tips you over: PTSD Part 1". All in the Mind. Australian Broadcasting Commission. 9 October 2004. Archived from the original on 3 June 2008.
^ Andreasen, Nancy C. (Feb 19, 2004). Brave New Brain: Conquering Mental Illness in the Era of the Genome. New York: Oxford University Press. p. 303. ISBN 978-0-19-516728-3.
^ Jones, Joshua A. 2013, VOL. 5 NO. 02 pp. 1–3. "Nostalgia to Post-Traumatic Stress Disorder: A Mass Society Theory of Psychological Reactions to Combat" Archived 2014-02-17 at the Wayback Machine The International Student Journal
^ "Henry IV, Part I, Act II, Scene 3 : |: Open Source Shakespeare". Opensourceshakespeare.org. Archived from the original on 2014-03-27. Retrieved 2014-01-30.
^ Shay, Jonathan (1994). Achilles in Vietnam: Combat Trauma and the Undoing of Character. Scribner. pp. 165–66.
^ World War One – A New Kind of War | Part II Archived 2016-03-03 at the Wayback Machine, From 14 – 18 Understanding the Great War, by Stéphane Audoin-Rouzeau, Annette Becker[incomplete short citation]
^ Möbius, Sascha (2015). "Im Kugelhagel der Musketen". Damals (in German). Vol. 47 no. 12. pp. 64–69.
^ "Ancient Assyrian Soldiers Were Haunted by War, Too".
^ Shay, J. (2000). "Killing rage: physis or nomos—or both" pp. 31–56 in War and Violence in Ancient Greece. Duckworth and the Classical Press of Wales.
ISBN 0715630466
^ "Civilian PTSD Symptoms and Risk for Involvement in the Criminal Justice System". Journal of the Academy of Psychiatry and the Law. 40 (4): 522–529. 2012-12-01. ISSN 1093-6793. Retrieved 2014-11-29.
^ Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB (December 1995). "Posttraumatic stress disorder in the National Comorbidity Survey". Archives of General Psychiatry. 52 (12): 1048–60. doi:10.1001/archpsyc.1995.03950240066012. PMID 7492257. Archived from the original on 2014-12-04.
^ Holmstrom LL, Burgess AW (1978). The Victim of Rape: Institutional Reactions. Wiley-Interscience. ISBN 978-0471407850.
^ Scrignar, C.B. "PTSD, the Traumatic Principle and Lawsuits". Psychiatric Times. Retrieved 2018-06-25.
^ "Search results: 'post-traumatic stress disorder' in the title of a journal article". U.S. National Library of Medicine. Archived from the original on 14 May 2016. Retrieved 21 January 2015.
^ "PTSD". TheFreeDictionary.com. Farlex, Inc. Retrieved 21 January 2015.
^ Thompson, Mark (2011). "The Disappearing 'Disorder': Why PTSD is becoming PTS". Time. Retrieved 3 October 2018.
^ Fodor KE, Unterhitzenberger J, Chou CY, Kartal D, Leistner S, Milosavljevic M, Nocon A, Soler L, White J, Yoo S, Alisic E (2014). "Is traumatic stress research global? A bibliometric analysis". European Journal of Psychotraumatology. 5 (1): 23269. doi:10.3402/ejpt.v5.23269. PMC 3930940. PMID 24563730.
^ ab Ojo JO, Greenberg MB, Leary P, Mouzon B, Bachmeier C, Mullan M, Diamond DM, Crawford F (December 2014). "Neurobehavioral, neuropathological and biochemical profiles in a novel mouse model of co-morbid post-traumatic stress disorder and mild traumatic brain injury". Frontiers in Behavioral Neuroscience. 8: 213. doi:10.3389/fnbeh.2014.00213. PMC 4067099. PMID 25002839.
^ Poulos AM, Reger M, Mehta N, Zhuravka I, Sterlace SS, Gannam C, Hovda DA, Giza CC, Fanselow MS (August 2014). "Amnesia for early life stress does not preclude the adult development of posttraumatic stress disorder symptoms in rats". Biological Psychiatry. 76 (4): 306–14. doi:10.1016/j.biopsych.2013.10.007. PMC 3984614. PMID 24231200.
^ Emerson A, Ponté L, Jerome L, Doblin R (2014). "History and future of the Multidisciplinary Association for Psychedelic Studies (MAPS)". Journal of Psychoactive Drugs. 46 (1): 27–36. doi:10.1080/02791072.2014.877321. PMID 24830183.
^ "A Manual for MDMA-Assisted Psychotherapy in the Treatment of Posttraumatic Stress Disorder" (PDF). Multidisciplinary Association for Psychedelic Studies. 4 January 2013. Archived from the original (PDF) on 2014-09-12. Retrieved 31 May 2014.
^ Philipps, Dave (2016-11-29). "F.D.A. Agrees to New Trials for Ecstasy as Relief for PTSD Patients". The New York Times. ISSN 0362-4331. Archived from the original on 2017-01-06. Retrieved 2017-01-12.
^ Amoroso T, Workman M (July 2016). "Treating posttraumatic stress disorder with MDMA-assisted psychotherapy: A preliminary meta-analysis and comparison to prolonged exposure therapy". Journal of Psychopharmacology. 30 (7): 595–600. doi:10.1177/0269881116642542. PMID 27118529.
^ "MAPS – Fear Extinction Learning with MDMA: Institutional Review Board Approves First Protocol Amendment". MAPS. Archived from the original on 2017-01-12. Retrieved 2017-01-12.
^ "MDMA-Assisted Psychotherapy". MAPS - Breakthrough for Psychedelic Medicine. Retrieved 2018-12-22.
^ de Kleine RA, Rothbaum BO, van Minnen A (October 2013). "Pharmacological enhancement of exposure-based treatment in PTSD: a qualitative review". European Journal of Psychotraumatology. 4: 21626. doi:10.3402/ejpt.v4i0.21626. PMC 3800126. PMID 24147208.
External links
| Classification | D
|
|---|---|
| External resources |
|
| Wikiquote has quotations related to: Posttraumatic stress disorder |
| Wikimedia Commons has media related to Posttraumatic stress disorder. |
Posttraumatic stress disorder at Curlie
- Post traumatic stress disorder information from The National Child Traumatic Stress Network
- Information resources from The University of Queensland School of Medicine
- APA practice parameters for assessment and treatment for PTSD (Updated 2017)
- Resources for professionals from the VA National PTSD Center
 Psychiatry portal
Psychiatry portal
