Diastole
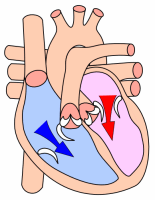
Heart performance during ventricular diastole: early diastole is a suction mechanism that draws blood 'down' from the left atrium (pink) and right atrium (blue) into each of the two ventricles. Then, in late ventricular diastole, the two atrial chambers begin to contract (atrial systole), forcing additional blood flow into the ventricles.
Diastole /daɪˈæstəliː/ is the part of the cardiac cycle during which the heart refills with blood after the emptying done during systole (contraction). Ventricular diastole is the period during which the two ventricles are relaxing from the contortions of contraction, then dilating and filling; atrial diastole is the period during which the two atria likewise are relaxing, dilating, and filling. The term diastole originates from the Greek word διαστολή, meaning dilation.[1]
Contents
1 Role in cardiac cycle
1.1 Early ventricular diastole
1.2 Late ventricular diastole
1.3 Atrial diastole
2 Diastolic pressure
3 Clinical notation
4 Diagnostic value
5 Effects of impaired diastolic function
6 See also
7 References
8 External links
Role in cardiac cycle
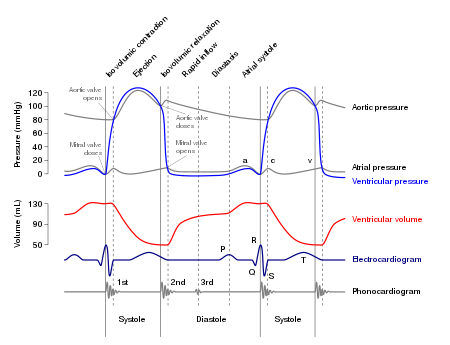
A Wiggers diagram, showing various events during diastole. During early ventricular diastole—see vertical bar marked "Isovolumetric relaxation"—pressure in each ventricle (light-blue trace) begins to drop quickly from the wave height reached during systole. When ventricular pressures fall below those in the atrial chambers the atrioventricular (mitral and tricuspid) valves open, causing blood volume (red trace) in the atria to flow into the ventricles. + In late ventricular diastole, the two atrial chambers begin to contract (atrial systole), causing blood pressure in both atria to increase and forcing additional blood volume into the ventricles. This beginning of the atrial systole is known as the atrial kick—see "Ventricular volume" trace (red) directly above the P-wave in the electrocardiogram trace (dark-blue).
For a healthy human heart the entire cardiac cycle typically runs less than one second. That is, for a typical heart rate of 75 beats per minute (bpm), the cycle requires 0.3 sec in ventricular systole (contraction)—pumping blood to all body systems from the two ventricles; and 0.5 sec in diastole (dilation), re-filling the four chambers of the heart, for a total time of 0.8 sec to complete the entire cycle.[2]
Early ventricular diastole
During early ventricular diastole, pressure in the two ventricles begins to drop from the peak reached during systole. When pressure in the left ventricle falls below that in the left atrium the mitral valve opens due to a negative pressure differential (suction) between the two chambers, causing blood in the atrium (accumulated during atrial diastole) to flow into the ventricle (see graphic at top). Likewise, the same phenomenon runs simultaneously in the right ventricle and right atrium through the tricuspid valve.
The ventricular filling flow (or flow from the atria into the ventricles) has an early (E) diastolic component caused by ventricular suction, and then a late one created by atrial systole (A). The E/A ratio is used as a diagnostic measure as its diminishment indicates probable diastolic dysfunction.[3]
Late ventricular diastole
Early diastole is a suction mechanism between the atrial and ventricular chambers.[4] Then, in late ventricular diastole, the two atrial chambers contract (atrial systole), causing blood pressure in both atria to increase and forcing additional blood flow into the ventricles. This beginning of the atrial systole is known as the atrial kick—see Wiggers diagram. The atrial kick does not supply the larger amount of flow (during the cardiac cycle) as about 80 per cent of the collected blood volume flows into the ventricles during the active suction period.[5]
Atrial diastole
At the beginning of the cardiac cycle, all four chambers of the heart—two atria and two ventricles—are in relaxation and dilation, or diastole. The atria are filling with separate blood volumes returning to the right atrium (from the vena cavae) and to the left atrium (from the lungs). After chamber and back pressures equalize, the mitral and tricuspid valves open, and the 'return' blood flows are passed through the atria into the ventricles. When the ventricles have completed most of their filling, the atria begin to contract (atrial systole), forcing blood under pressure into the ventricles. Now the ventricles start to contract, and as pressures within the ventricles rise, the mitral and tricuspid valves are closed.
As pressures within the ventricles continue to rise, they exceed the 'back pressures' in the aorta trunk and the pulmonary arteries trunk, and the aortic and pulmonary valves open—and now blood is ejected from the heart. Ejection causes pressure within the ventricles to fall, and, simultaneously, the atria begin to refill (atrial diastole). Finally, pressures within the ventricles fall below the back pressures in the trunks of the aorta and the pulmonary arteries, and the aortic and pulmonary valves close. The ventricles start to relax, the mitral and tricuspid valves begin to open, and the cycle begins again.[6]
In summary, when the ventricles are in systole and contracting, the atria are relaxed and collecting blood as 'return' flows. When, in late diastole, the ventricles become fully dilated, the atria begin to contract, pumping blood to the ventricles. The atria feed a steady supply of blood to the ventricles, thereby serving as a reservoir to the ventricles and ensuring that these pumps never run dry.[7] This coordination ensures that blood is pumped and circulated efficiently throughout the body.[8]
Diastolic pressure
Here the adjective "diastolic" refers to the function (the "diastolic function") of filling the heart with blood between muscle contractions; it describes that portion of the cardiac cycle opposite to contraction. The term is more commonly known as one of the two main components for measuring blood pressure—namely, "diastolic pressure" refers to the lowest pressure in the arterial bloodstream occurring during each heartbeat. (The other component is "systolic pressure", which is the highest arterial pressure during each heartbeat.)
Clinical notation
When blood pressure is stated for medical purposes, it is usually written with the systolic and diastolic pressures separated by a slash, for example, 120/80 mmHg. This clinical notation is not a mathematical figure for a fraction or ratio, nor a display of a numerator over a denominator. Rather it is a medical notation showing the two clinically significant pressures involved (i.e., systolic-slash-diastolic, or 120/80). It is often shown followed by a third number, the value of the heart rate (in beats per minute), which typically is measured jointly with blood pressure readings.
Diagnostic value
Examining diastolic function during a cardiac stress test is a good way to test for heart failure with preserved ejection fraction.[9]
Classification of Blood Pressure in Adults[10]
| Blood Pressure Classification | Systolic BP (mmHg) | Diastolic BP (mmHg) |
|---|---|---|
| Optimal | <120 | and <80 |
| Prehypertension | 120–139 | or 80–89 |
| Stage 1 Hypertension | 140–159 | or 90–99 |
| Stage 2 Hypertension | ≥160 | or ≥100 |
Effects of impaired diastolic function
Brain natriuretic peptide (BNP) is a cardiac neurohormone secreted from ventricular myocytes (ventricular muscle cells) at the end of diastole—this in response to the normal, or sub-normal (as the case may be), stretching of cardiomyocytes (heart muscle cells) during systole. Elevated levels of BNP indicate excessive natriuresis (excretion of sodium to the urine) and decline of ventricular function, especially during diastole. Increased BNP concentrations have been found in patients who experience diastolic heart failure.[11]
Impaired diastolic function can result from the decreased compliance of ventricular myocytes, and thus the ventricles, which means the heart muscle does not stretch as much as needed during filling.[2] This will result in a reduced end diastolic volume (EDV) and, according to the Frank-Starling mechanism, a reduced EDV will lead to a reduced stroke volume, thus a reduced cardiac output. Over time, decreased cardiac output will diminish the ability of the heart to circulate blood efficiently throughout the body.
See also
- Systole (medicine)
- Blood pressure
- Wiggers diagram
References
^ Diastole. Merriam-Webster Online Dictionary. 24 August 2008.
^ ab Widmaier, Eric P. (2014). Vander's Human Physiology: The Mechanisms of Body Function, 13/e. McGraw Hill Education. p. 378..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output .citation q{quotes:"""""""'""'"}.mw-parser-output .citation .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .citation .cs1-lock-limited a,.mw-parser-output .citation .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .citation .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-ws-icon a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/4/4c/Wikisource-logo.svg/12px-Wikisource-logo.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-maint{display:none;color:#33aa33;margin-left:0.3em}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ Mohamed, A. L.; Yong, J; Masiyati, J; Lim, L; Tee, S. C. (2004). "The prevalence of diastolic dysfunction in patients with hypertension referred for echocardiographic assessment of left ventricular function". The Malaysian Journal of Medical Sciences. 11 (1): 66–74. PMC 3438153. PMID 22977362.
^ Sabbah, H. N.; Stein, P. D. (1981). "Pressure-diameter relations during early diastole in dogs. Incompatibility with the concept of passive left ventricular filling". Circulation Research. 48 (3): 357–65. doi:10.1161/01.RES.48.3.357. PMID 7460209.
^ Williams, Gareth. Advanced Biology for You.
[page needed][full citation needed]
^ Hall, John (2011). Guyton and Hall textbook of medical physiology (12th ed.). Philadelphia, Pa.: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
^ Topol, Eric J (2000). Cleveland Clinic Heart Book. New York: Hyperion. pp. 4–5. ISBN 978-0-7868-6495-9.
^ Betts, J. Gordon (2013). Anatomy & physiology. pp. 787–846.
ISBN 1-938168-13-5.
^ Erdei T, Aakhus S, Marino P, Paulus WJ, Smiseth OA, Fraser AG (2015). "Pathophysiological rationale and diagnostic targets for diastolic stress testing". Heart. 101 (17): 1355–60. doi:10.1136/heartjnl-2014-307040. PMID 26001845.
^ "The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure" (PDF).
^ Eroglu, Serpil; Bozbas, Huseyin; Muderrisoglu, Haldun (2008). "Diagnostic value of BNP in diastolic heart failure". Biochemia Medica: 183–92. doi:10.11613/bm.2008.018.
External links
| Look up diastole in Wiktionary, the free dictionary. |
